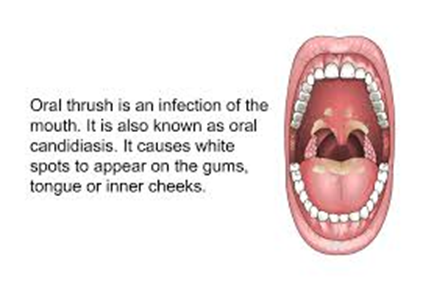
Oral candidiasis, also known as oral
thrush among other names, is candidiasis that occurs in the mouth. That
is, oral candidiasis is a mycosis (yeast/fungal infection)
of Candidas pieces on the mucous membranes of
the mouth.
Candida albicans is
the most implicated organism in this condition. C. albicans is
carried in the mouths of about 50% of the world's population as a normal
component of the oral microbiota. This candida carriage state is not
considered a disease, but when Candida species become
pathogenic and invade host tissues, oral candidiasis can occur. This change
usually constitutes an opportunistic infection by normally harmless micro-organisms because of
local (i.e., mucosal) or systemic factors altering host immunity.
Oral candidiasis is a mycosis (fungal
infection). Traditionally, oral candidiasis is classified using the Lehner
system, originally described in the 1960s, into acute and chronic forms (see
table). Some of the subtypes always occur as acute (e.g., acute
pseudomembranous candidiasis), and others chronic. However, these typical
presentations do not allow Pseudomembranous
Acute pseudomembranous candidiasis is a classic form of oral
candidiasis, commonly referred to as thrush. Overall, this is the most common
type of oral candidiasis, accounting for about 35% of oral candidiasis cases.
It is characterized by a coating or individual patches of
pseudomembranous white slough that can be easily wiped away to reveal
erythematous (reddened), and sometimes minimally bleeding, mucosa beneath. These areas of pseudo membrane are sometimes
described as "curdled milk", or "cottage cheese". The white material is made up of debris,
fibrin, and desquamated epithelium that has been invaded by yeast cells and
hyphae that invade to the depth of the stratum spinosum. As an erythematous surface is revealed beneath
the pseudo membranes, some consider pseudomembranous candidiasis and
erythematous candidiasis stages of the same entity. Some sources state that if there is bleeding
when the pseudo membrane is removed, then the mucosa has likely been affected
by an underlying process such as lichen planus or chemotherapy. Pseudomembranous candidiasis can involve any
part of the mouth, but usually it appears on the tongue, buccal mucosae or
palate.
It is classically an acute condition, appearing in infants, people taking antibiotics or immunosuppressant medications, or immunocompromising diseases. However, sometimes it can be chronic and intermittent, even lasting for many years. Chronicity of this subtype occurs in immunocompromised states, (e.g., leukemia, HIV) or in persons who use corticosteroids topically or by aerosol. Acute and chronic prepays hold true, which created problems with this system. A more recently proposed classification of oral candidiasis distinguishes primary oral candidiasis, where the condition is confined to the mouth and perioral tissues, and secondary oral candidiasis, where there is involvement of other parts of the body in addition to the mouth. The global human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) pandemic has been an important factor in the move away from the traditional classification since it h
as led to the formation of a new group of patients who present with atypical forms of oral candidiasis.
By appearance
Three main clinical appearances of candidiasis are generally
recognized: pseudomembranous, erythematous (atrophic) and hyperplastic. Most often, affected individuals display one
clear type or another, but sometimes there can be more than one clinical
variant in the same person.
Pseudomembranous.
Acute pseudomembranous candidiasis is a classic form of oral
candidiasis, commonly referred to as thrush. Overall, this is the most
common type of oral candidiasis, accounting for about 35% of oral candidiasis
cases.
It is characterized by a coating or individual patches of
pseudomembranous white slough that can be easily wiped away to reveal erythematous (reddened),
and sometimes minimally bleeding, mucosa beneath. These areas of pseudo
membrane are sometimes described as "curdled milk", or
"cottage cheese". The white material is made up of debris, fibrin, and desquamated epithelium that has
been invaded by yeast cells and hyphae that invade to the depth of the stratum
spinosum.[4] As an
erythematous surface is revealed beneath the pseudo membranes, some consider
pseudomembranous candidiasis and erythematous candidiasis stages of the same
entity. Some sources state that if there is bleeding when the pseudo
membrane is removed, then the mucosa has likely been affected by an underlying
process such as lichen planus or chemotherapy. Pseudomembranous candidiasis can involve any
part of the mouth, but usually it appears on the tongue, buccal mucosae or
palate.
It is classically an acute condition, appearing in infants,
people taking antibiotics or immunosuppressant medications, or
immunocompromising diseases. However, sometimes it can be chronic and intermittent,
even lasting for many years. Chronicity of this subtype generally occurs
in immunocompromised states,
(e.g., leukemia, HIV) or in
persons who use corticosteroids topically or by aerosol. Acute and chronic
pseudomembranous candidiasis are indistinguishable in appearance.
Erythematous.
Erythematous (atrophic) candidiasis is when the condition
appears as a red, raw-looking lesion.[8] Some sources
consider denture-related stomatitis, angular stomatitis, median rhomboid
glossitis, and antibiotic-induced stomatitis as subtypes of erythematous
candidiasis, since these lesions are commonly erythematous/atrophic. It may
precede the formation of a pseudo membrane, be left when the membrane is
removed, or arise without prior pseudo membranes. Some sources state that
erythematous candidiasis accounts for 60% of oral candidiasis cases. Where
it is associated with inhalation steroids (often used for treatment of ,
erythematous candidiasis commonly appears on the palate or the dorsum of the
tongue. On the tongue, there is loss of the lingual papillae (depopulation),
leaving a smooth area.
Acute erythematous candidiasis usually occurs on the dorsum of
the tongue in persons taking long term corticosteroids or antibiotics, but
occasionally it can occur after only a few days of using a topical antibiotics. This
is usually termed "antibiotic sore mouth", "antibiotic sore
tongue", or "antibiotic-induced stomatitis" because it is
commonly painful as well as red.
Chronic erythematous candidiasis is more usually associated with
denture wearing (see denture-related stomatitis).
Hyperplastic.
This variant is also sometimes termed "plaque-like
candidiasis" or "nodular candidiasis". The most common appearance of
hyperplastic candidiasis is a persistent white plaque that does not rub off.
The lesion may be rough or nodular in texture. Hyperplastic candidiasis is
uncommon, accounting for about 5% of oral candidiasis cases, and is
usually chronic and found in adults. The most common site of involvement is the
commissural region of the buccal
mucosa, usually on both sides of the mouth.
Another term for hyperplastic candidiasis is "candida
leukoplakia". This term is a largely historical synonym for this subtype
of candidiasis, rather than a true leukoplakia. Indeed, it can be
clinically indistinguishable from true leukoplakia, but tissue biopsy shows candida
hyphae invading the epithelium. Some sources use this term to describe
leukoplakia lesions that become colonized secondarily by Candida species,
thereby distinguishing it from hyperplastic candidiasis It is known
that Candida resides more readily in mucosa that is altered,
such as may occur with dysplasia and hyperkeratosis in an area of leukoplakia.
Associated lesions
Candida-associated lesions are primary oral candidiasis
(confined to the mouth), where the causes are thought to be multiple.[4] For example,
bacteria as well as Candida species may be involved in these
lesions. Frequently, antifungal therapy
alone does not permanently resolve these lesions, but rather the underlying
predisposing factors must be addressed, in addition to treating the
candidiasis.
Angular cheilitis.
Angular cheilitis
Main article: Angular cheilitis
Angular cheilitis is inflammation at the corners (angles) of the
mouth, very commonly involving Candida species, when sometimes
the terms "Candida-associated angular cheilitis", or less
commonly "monilial perlèche" are used. Candida organisms
alone are responsible for about 20% of cases, and a mixed infection
of C. albicans and Staphylococcus aureus for about 60% of
cases. Signs and symptoms include soreness, (redness), and
fissuring of one, or more commonly both the angles of the mouth, with edema
(swelling) seen intraorally on the commissures (inside the corners of the
mouth). Angular cheilitis generally occurs in elderly people and is associated
with denture related stomatitis.[13]
Denture-related stomatitis
Main article: Denture-related stomatitis
This term refers to a mild inflammation and erythema of the
mucosa beneath a denture, usually an upper
denture in elderly edentulous individuals
(with no natural teeth remaining). Some report that up to 65% of denture
wearers have this condition to some degree. About 90% of cases are associated with Candida species, where
sometimes the terms "Candida-associated denture
stomatitis", or
"Candida-associated denture-induced stomatitis" (CADIS), are
used. Some sources state that this is by far the most common form of oral
candidiasis. Although this condition is also known as "denture sore
mouth", there is rarely any pain. Candida is associated
with about 90% of cases of denture related stomatitis.
Median rhomboid glossitis
Main article: Median rhomboid glossitis
This is an elliptical or rhomboid lesion in the center of the
dorsal tongue, just anterior (in front) of the circumvallate papillae. The area is depopulated, reddened
(or red and white) and rarely painful. There is frequently Candida species
in the lesion, sometimes mixed with bacteria.
Linear gingival erythema
Main article: Linear gingival erythema
This is a localized or generalized, linear band of
erythematous gingivitis (inflammation of
the gums). It was first observed in HIV infected individuals and termed
"HIV-gingivitis", but the condition is not confined to this group.
Others
Chronic multifocal oral candidiasis
This is an uncommon form of chronic (more than one month in
duration) candida infection involving multiple areas in the mouth, without
signs of candidiasis on other mucosal or cutaneous sites. The lesions are
variably red and/or white. Unusually for candida infections, there is an
absence of predisposing factors such as immunosuppression, and it occurs in healthy
individuals, normally elderly males. Smoking is a known risk factor.
Chronic mucocutaneous candidiasis
Main article:
This refers to a group of rare syndromes characterized by
chronic candida lesions on the skin, in the mouth and on other mucous membranes
(i.e., a secondary oral candidiasis). These include Localized chronic
mucocutaneous candidiasis, diffuse mucocutaneous candidiasis (Candida
granuloma), candidiasis–endocrinopathy syndrome and candidiasis thymoma
syndrome. About 90% of people with chronic mucocutaneous candidiasis have
candidiasis in the mouth.
Signs and symptoms
Signs and symptoms are dependent upon the type of oral
candidiasis. Often, apart from the appearance of the lesions, there are usually
no other signs or symptoms. Most types of oral candidiasis are painless, but a
burning sensation may occur in some cases. Candidiasis can, therefore,
sometimes be misdiagnosed as burning mouth syndrome. A burning
sensation is more likely with erythematous (atrophic) candidiasis, whilst
hyperplastic candidiasis is normally entirely asymptomatic. Acute atrophic
candidiasis may feel like the mouth has been scalded with a hot
liquid. Another potential symptom is a metallic, acidic, salty or bitter
taste in the mouth. The pseudomembranous type rarely causes any symptoms
apart from possibly some discomfort or bad taste due to the presence of the
membranes. Sometimes the patient describes the raised pseudo
membranes as "blisters." Occasionally there can be dysphagia (difficulty
swallowing), which indicates that the candidiasis involves the oropharynx or the esophagus, as well as
the mouth. The trachea and the larynx may also be
involved where there is oral candidiasis, and this may cause hoarseness of the
voice.
Causes
Species
The causative organism is usually Candida albicans, or less
commonly other Candida species such as (in decreasing order of frequency) Candida
tropicalis[ Candida glabrata, Candida
parasitosis,] Candida krusei, or other
species (Candida
stellated, Candida pleiotropically
Candida fermata, Candida rugosa, Candida
eroticism, Candida
sublimeness, and C.
albicans accounts for about 50% of oral candidiasis cases, and
together C. albicans, C. tropicalis and C.
glabrata account for over 80% of cases. Candidiasis caused by non-C. albicans Candida
(NCAC) species is associated more with immunodeficiency. For example, in HIV/AIDS, C.
sublimeness and C. eroticism can become pathogenic. About
35-50% of humans possess C. albicans as part of their normal oral microbiota. With more sensitive detection
techniques, this figure is reported to rise to 90%.[6] This candida
carrier state is not considered a disease, since there are no
lesions or symptoms of any kind. Oral carriage of Candida is
pre-requisite for the development of oral candidiasis. For Candida species
to colonize and survive as a normal component of the oral microbiota, the
organisms must be capable of adhering to the epithelial surface of
the mucous membrane lining the
mouth.[19] This adhesion
involves adhesins (e.g., hyphal wall protein 1), and extracellular
polymeric materials (e.g., mannoprotein). Therefore, strains of Candida with
more adesion capability have more pathogenic potential than other
strains. The prevalence of Candida carriage varies with geographic
location, and many other factors. Higher carriage is reported during the
summer months, in females, in hospitalized individuals, in persons
with blood group O and in non-secretors of blood group antigens in saliva. Increased rates of Candida carriage
are also found in people who eat a diet high in carbohydrates, people who wear
dentures, people with xerostomia (dry mouth), in people taking broad spectrum
antibiotics, smokers, and in immunocompromised individuals (e.g., due to
HIV/AIDS, diabetes, cancer, Down
syndrome or malnutrition). Age also influences oral carriage,
with the lowest levels occurring in newborns, increasing dramatically in
infants, and then decreasing again in adults. Investigations have quantified
oral carriage of Candida albicans at 300-500 colony
forming units in healthy
persons. More Candida is detected in the early morning
and the late afternoon. The greatest quantity of Candida species
are harbored on the posterior dorsal tongue,[13] followed by
the palatal and the buccal mucosae. Mucosa covered by an oral appliance
such as a denture harbors significantly more candida species than uncovered
mucosa.
When Candida species cause lesions - the result
of invasion of the host tissues - this is termed candidiasis.
Some consider oral candidiasis
a change in the normal oral environment rather than an exposure or true
"infection" as such. The exact process by which Candida species
switch from acting as normal oral commensals (saprophytic) state in the carrier
to acting as a pathogenic organism (parasitic state) is not
), which is thought to be relatively harmless; and a hyphal form
associated with invasion of host tissues. Apart from true hyphae, Candida can
also form pseudo hyphae — elongated filamentous cells, lined end to end.[4] As a general
ru completely understood.
Several Candida species are polymorph genic, that is,
capable of growing in different forms depending on the environmental
conditions. C. albicans can appear as a yeast form (blastosporesis, candidiasis
presenting with white lesions is mainly caused by Candida species
in the hyphal form and red lesions by yeast forms. C. albicans and C.
sublimeness are also capable of forming germ tubes (incipient hyphae)
and chlamydospores under the right conditions. C. albicans is
categorized serologically into A or B serotypes. The prevalence is roughly
equal in healthy individuals, but type is more prevalent in immunocompromised
individuals.
Predisposing factors. The host defenses against
opportunistic infection of candida species are
·
The oral epithelium, which acts both as a physical barrier
preventing micro-organisms from entering and the tissues and is the site of
cell mediated immune reactions.
·
Competition and inhibition interactions between candida
species and other micro-organisms in the mouth, such as the many hundreds of various
kinds of bacteria.
·
Saliva, which possesses
both mechanical cleansing action and immunologic action, including salivary immunoglobulin A antibodies,
which aggregate candida organisms and prevent them adhering to the epithelial
surface; and enzymatic components
such as lysozyme, lactoperoxidase and
antileukoprotease.
Disruption to any of these local and systemic host defense
mechanisms constitutes a potential susceptibility to oral candidiasis, which
rarely occurs without predisposing factors.[4] It is often
described as being "a disease of the diseased",[2][4] occurring in
the very young, the very old, or the very sick.
Oral candidiasis in an infant. At
very young ages, the immune system is yet to develop fully.
Immunodeficiency
Immunodeficiency is a state of
reduced function of the immune system, which can be caused by medical
conditions or treatments.
Acute pseudomembranous candidiasis occurs in about 5% of newborn infants.[9] Candida
species are acquired from the mother's vaginal canal during
birth. At very young ages, the immune system is yet to develop fully and there
is no individual immune response to candida species,[9] an infants
antibodies to the fungus are normally supplied by the mother's breast milk.
Other forms of immunodeficiency which may cause oral candidiasis
include HIV/AIDS, active and
treatment, chemotherapy or radiotherapy.
Corticosteroid medications may
contribute to the appearance of oral candidiasis, as they cause suppression
of immune function either systemically or on a local/mucosal level, depending
on the route of administration. Topically administered corticosteroids in the
mouth may take the form of mouthwashes, dissolving lozenges or mucosal gels;
sometimes being used to treat various forms of stomatitis.
Systemic corticosteroids may also result in candidiasis.
Inhaled corticosteroids (e.g., for treatment of asthma or chronic obstructive pulmonary disease), are not intended
to be administered topically in the mouth, but inevitably there is contact with
the oral andof the erythematous variety. Candidiasis appears at the sites
where the steroid has contacted the mucosa, typically the dorsum of the tongue
(median rhomboid glossitis) and sometimes also on the palate. Candida lesions on both sites are sometimes
termed "kissing lesions because they approximate when the tongue is
in contact with the palate.
Denture wearing
Denture wearing and
poor denture hygiene, particularly wearing the denture continually rather than
removing it during sleep,[3] is another
risk factor for both candida carriage and oral candidiasis. Dentures provide a
relative acidic, moist and anaerobic environment because the mucosa covered by
the denture is sheltered from oxygen and saliva. Loose, poorly fitting
dentures may also cause minor trauma to the mucosa, ] which is
thought to increase the permeability of the mucosa and increase the ability
of C. albicans to invade the tissues. These conditions all favor
the growth of C. albicans. Sometimes dentures become very worn, or
they have been constructed to allow insufficient lower facial height (occlusal
vertical dimension), leading to over-closure of the mouth (an appearance
sometimes described as "collapse of the jaws"). This causes deepening
of the skin folds at the corners of the mouth (nasolabial crease), in effect
creating intertriginous areas where
another form of candidiasis, angular cheilitis, can develop. Candida species can
adhere to the surface of dentures, most of which are made from polymethyl
acrylate. They exploit micro-fissures and cracks in the surface of dentures to
aid their retention. Dentures may therefore become covered in a biofilm, and act as
reservoirs of infection, continually re-infecting the mucosa. For this
reason, disinfecting the denture is a vital part of treatment of oral
candidiasis in persons who wear dentures, as well as correcting other factors
like inadequate lower facial height and fit of the dentures.
Dry mouth
Both the quantity and quality of saliva are important oral
defenses against candida. Decreased salivary flow rate or a change in the
composition of saliva, collectively termed salivary hypofunction or hyposalivation
is an important predisposing factor. Xerostomia is frequently
listed as a cause of candidiasis, but xerostomia can be subjective or objective,
i.e., a symptom present with or without actual changes in the saliva
consistency or flow rate.
Malnutrition, whether
by malabsorption, or poor diet,
especially hematinic deficiencies (iron, vitamin B12, folic acid)
can predispose to oral candidiasis, by causing diminished host
defense and epithelial integrity. For example, iron deficiency anemia is thought to cause
depressed cell-mediated immunity. Some sources state that deficiencies
of vitamin A or pyridoxine are also linked.
There is limited evidence that a diet high in carbohydrates predisposes to oral
candidiasis. In studies it shows that Candida
growth, adhesion and biofilm formation is enhanced by the presence of carbohydrates
such as glucose, galactose and sucrose.
Smoking
Smoking especially heavy
smoking, is an important predisposing factor but the reasons for this
relationship are unknown. One hypothesis is that cigarette smoke contains
nutritional factors for C. albicans, or that local epithelial
alterations occur that facilitate colonization of candida species.
Antibiotics
Broad-spectrum antibiotics (e.g. tetracycline) eliminate the
competing bacteria and disrupt the normally balanced ecology of oral
microorganisms, ich can cause antibiotic-induced candidiasis
Other factors
Several other factors can contribute to infection, including endocrine
disorders (e.g. diabetes when poorly
controlled), and/or the presence of certain other mucosal lesions, especially
those that cause hyperkeratosis and/or dysplasia (e.g. lichen
planus). Such changes in the
mucosa predispose it to secondary infection with candidiasis. Other
physical mucosal alterations are sometimes associated with candida overgrowth,
such as fissured tongue (rarely), tongue piercing, atopy, and/or hospitalization.
Diagnosis
The diagnosis can typically be made from the clinical appearance
alone, but not always. As candidiasis can be variable in appearance, and
present with white, red or combined white and red lesions, the differential diagnosis can be
extensive. In pseudomembranous candidiasis, the membranous slough can be wiped
away to reveal an erythematous surface underneath. This is helpful in distinguishing pseudomembranous
candidiasis from other white lesions in the mouth that cannot be wiped away,
such as lichen planus, oral hairy leukoplakia. Erythematous
candidiasis can mimic geographic
tongue. Erythematous candidiasis usually has
a diffuse border that helps distinguish it from erythrolein, which
normally has a sharply defined border.
Special investigations to detect the presence of candida species
include oral swabs, oral rinse or oral smears.[31] Smears are
collected by gentle scraping of the lesion with a spatula or tongue blade and
the resulting debris directly applied to a glass slide. Oral swabs are taken if
culture is required. Some recommend that swabs be taken from 3 different oral
sites. Oral rinse involves rinsing the mouth with
phosphate-buffered saline for 1 minute and then spitting the solution into
a vessel that examined in a pathology laboratory. Oral rinse technique can
distinguish between commensal candida carriage and candidiasis. If candida
leukoplakia is suspected, a biopsy may be indicated.. Smears and biopsies
are usually stained with periodic
acid-Schiff, which stains
carbohydrates in fungal cell walls in magenta. Gram staining is also used
as Candida stains are strongly Gram positive.
Sometimes an underlying medical condition is sought, and this
may include blood tests for full blood count and hematinic.
If a biopsy is taken, the histopathologic appearance can be
variable depending upon the clinical type of candidiasis. Pseudomembranous
candidiasis shows hyperplastic epithelium with a superficial parakeratotic
desquamating (i.e., separating) layer.[32] Hyphae
penetrate to the depth of the stratum spinosum, and appear as weakly basophilic
structures. Polymorphonuclear cells also infiltrate the
epithelium, and chronic inflammatory cells infiltrate the lamina propria.
Atrophic candidiasis appears as thin, atrophic epithelium, which
is non-keratinized. Hyphae are sparse, and inflammatory cell infiltration of
the epithelium and the lamina propria. In essence, atrophic candidiasis appears like
pseudomembranous candidiasis without the superficial desquamating layer.
Hyperplastic
candidiasis is variable. Usually there is hyperplastic and acanthotic
epithelium with parakeratosis. There is an inflammatory cell infiltrate and
hyphae are visible. Unlike other forms of candidiasis, hyperplastic candidiasis
may show dysplasia.
Oral candidiasis can be treated with topical anti-fungal drugs, such
as nystatin, miconazole, Gentian violet or amphotericin B. Surgical excision
of the lesions may be required in cases that do not respond to anti-fungal
medications.
Underlying immunosuppression may be medically manageable once it
is identified, and this helps prevent recurrence of candida infections.
Patients who are immunocompromised, either with HIV/AIDS or as a result
of chemotherapy, may require
systemic prevention or treatment with oral or intravenous administered
anti-fungal. However, there is strong evidence that drugs that are absorbed or
partially absorbed from the GI tract can prevent candidiasis more effectively
than drugs that are not absorbed in the same way.
If candidiasis is secondary to corticosteroid or antibiotic use,
then use may be stopped, although this is not always a feasible option.
Candidiasis secondary to the use of inhaled steroids may be treated by rinsing
out the mouth with water after taking the steroid.[15] Use of a
spacer device to reduce the contact with the oral mucosa may greatly reduce the
risk of oral candidiasis.
In recurrent oral candidiasis, the use of azole antifungals
risks selection and enrichment of drug-resistant strains of candida
organisms. Drug resistance is
increasingly more common and presents a serious problem in persons who are
immunocompromised.
Prophylactic use of
antifungals is sometimes employed in persons with HIV disease, during
radiotherapy, during immunosuppressive or prolonged antibiotic therapy as the
development of candida infection in these groups may be more serious.
The candida load in the mouth can be reduced by improving oral hygiene measures, such as
regular toothbrushing and use of anti-microbial mouthwashes. Since smoking is associated
with many of forms of oral candidiasis, cessation may be beneficial.
Denture hygiene
See also:
Good denture hygiene involves regular cleaning of the dentures
and leaving them out of the mouth during sleep. This gives the mucosa a chance
to recover, while wearing a denture during sleep is often likened to sleeping
in one's shoes. In oral candidiasis, the dentures may act as a reservoir of
Candida species known as denture stomatitis which continually reinfects
the mucosa once antifungal medication is stopped. Therefore, they must be
disinfected as part of the treatment for oral candidiasis. There are
commercial denture cleaner preparations
for this purpose, but it is readily accomplished by soaking the denture
overnight in a 1:10 solution of sodium
hypochlorite (Milton, or household bleach).[7] Bleach may
corrode metal components,[13] so if the
denture contains metal, soaking it twice daily in solution can be carried
out instead. An alternative method of disinfection is to use a 10% solution
of acetic acid (vinegar) as
an overnight soak, or to microwave the dentures in 200mL water for 3 minutes
at 650 watts. Microwave sterilization is only suitable if no metal
components are present in the denture. Antifungal medication can also be
applied to the fitting surface of the denture before it is put back in the
mouth. Other problems with the dentures, such as inadequate occlusal vertical
dimension may also need to be corrected in the case of angular cheilitis.
Prognosis
The severity of oral candidiasis is subject to great variability
from one person to another and in the same person from one occasion to the
next.[8] The prognosis
of such infection is usually excellent after the application of topical or
systemic treatments. However, oral candidiasis can be
recurrent. Individuals continue to be at risk of the condition if
underlying factors such as reduced salivary flow rate or immunosuppression are
not rectifiable.[8]
Candidiasis can be a marker for underlying disease, so the
overall prognosis may also be dependent upon this. For example, a transient
erythematous candidiasis that developed after antibiotic therapy usually
resolves after antibiotics are stopped (but not always immediately), and
therefore carries an excellent prognosis—but candidiasis may occasionally be a
sign of more sinister undiagnosed pathology, such as HIV/AIDS or leukemia.
It is possible for candidiasis to spread to/from the mouth, from
sites such as the pharynx, esophagus, lungs, liver, anogenital region, skin or
the nails. The read of
oral candidiasis to other sites usually occurs in debilitated individuals. It is also possible that candidiasis is spread
by sexual contact. Rarely, a superficial
candida infection such as oral candidiasis can cause invasive
candidiasis, and even prove
fatal. The observation that Candida species are normally harmless commensals on
the one hand, but are also occasionally capable of causing fatal invasive candidiasis
has led to the description "Dr Jekyll and Mr. Hyde".
The role of thrush in the hospital and ventilated patients is
not entirely clear, however, there is a theoretical risk of positive
interaction of candida with topical bacteria.
Epidemiology
In humans, oral candidiasis is the most common form of candidiasis, by
far the most common fungal infection of the mouth,[5] and it also
represents the most common opportunistic oral infection in humans[40] with lesions
only occurring when the environment favors pathogenic behavior.
Oropharyngeal candidiasis is common during cancer care, and it
is a very common oral sign in individuals with HIV. Oral candidiasis occurs in about two thirds of
people with concomitant AIDS and esophageal candidiasis.
The incidence of all forms of candidiasis have increased in
recent decades. This is due to developments in medicine, with more invasive
medical procedures and surgeries, more widespread use of broad-spectrum
antibiotics and immunosuppression therapies. The HIV/AIDs global pandemic has
been the greatest factor in the increased incidence of oral candidiasis since
the 1980s. The incidence of candidiasis caused by NCAC species is also
increasing, again thought to be due to changes in medical practice (e.g., organ transplantation and use of indwelling
catheters.
His
Oral candidiasis has been recognized throughout recorded history. The first description of this
condition is thought to have occurred in the 4th century B.C. in
"Epidemics" (a treatise that is part of the Hippocratic), where
descriptions of what sounds like oral candidiasis are stated to occur with
severe underlying disease.
The colloquial term "thrush" refers to the resemblance
of the white flecks present in some forms of candidiasis (e.g.,
pseudomembranous candidiasis), with the breast of the bird of the same name.
Society and culture
Many pseudoscientific claims by
proponents of alternative
medicine surround the topic
of candidiasis. Oral candidiasis is sometimes presented in this manner as a
symptom of a widely prevalent systemic candidiasis, candida
hypersensitivity syndrome, yeast allergy, or gastrointestinal candida
overgrowth, which are medically unrecognized conditions.
Jan
Rick Jennings, MHA, LFACHE
Senior
Consultant
Senior
Management Resources, LLC
JanJenningsBlog.Blogspot.com
412.913.0636
Cell
724.733.0509
Office






No comments:
Post a Comment