Lead Poisoning
Type of metal poisoning caused
by lead in the
body. The brain is the most
sensitive. Symptoms may include abdominal
pain, constipation, headaches,
irritability, memory problems, infertility, and tingling in the
hands and feet. It causes almost 10% of intellectual disability of
otherwise unknown cause and can result in behavioral problems. Some of the
effects are p. In severe
cases, anemia, seizures, coma, or death may occur..
Exposure to lead
can occur by co taminated air, water, dust, food, or consumer
products. Lead poisoning poses a significantly increased risk to children
as they are far more likely to ingest lead indirectly by chewing on toys or
other objects that are coated in lead paint. The amount of lead that can be absorbed by
children is also higher than that of adults. Exposure at work is a common cause
of lead poisoning in adults with certain occupations at particular
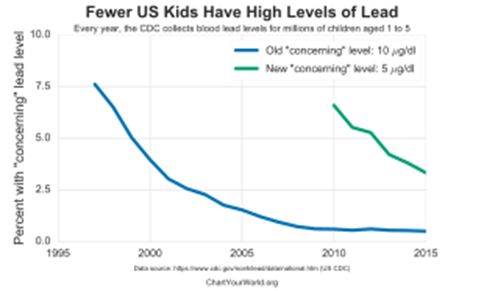
risk. Diagnosis is typically by measurement of the blood lead level. The Centers for Disease Control and Prevention (US) has
set the upper limit for blood lead for adults at 10 µg/dl (10 µg/100
g) and for children at 3.5 µg/dl, previously before October 2021 5 µg/d. Elevated
lead may also be detected by changes in red blood cells or dense
lines in the bones of children as seen on X-ray.
Lead poisoning is
preventable. This includes individual efforts such as
removing lead-containing items from the home,[ workplace
efforts such as improved ventilation and monitoring, state and
national policies that ban lead in products such as paint, gasoline,
ammunition, wheel weights, and fishing weights, reduce allowable levels in
water or soil, and provide for cleanup of contaminated soil. Workers' education could be
helpful as well. The major treatments are removal of the source
of lead and the use of medications that bind lead so it can be eliminated from the body, known as chelation therapy. Chelation
therapy in children is recommended when blood levels are greater than
40–45 µg/dl Medications used include dimercaprol, edetate calcium disodium, and succimer.
In 2016, lead is
believed to have resulted in 540,000 deaths worldwide. It occurs
most commonly in the developing
world.[2] There also
are numerous cases in the developed world, with there being thousands of
American communities with higher lead burdens than seen during the peak of
the Flint water crisis. Those who are poor are at greater risk. Lead is believed to result in 0.6% of the
world's disease burden.[5]According to a
study, half of the US population has been exposed to substantially detrimental
lead levels in early childhood – mainly from car exhaust whose lead pollution
peaked in the 1970s and caused widespread loss in cognitive ability.
People have been
mining and using lead for thousands of years. Descriptions of lead poisoning
date to at least 2000 BC, while efforts to limit lead's use
date back to at least the 16th century. Concerns for low levels of
exposure began in the 1970s with there being no safe threshold for lead
exposure.
Classification
Classically,
"lead poisoning" or "lead intoxication" has been defined as
exposure to high levels of lead typically associated with severe health
effects. Poisoning is a pattern of symptoms that occur
with toxic effects from mid to high levels of exposure; toxicity is a wider
spectrum of effects, including subclinical ones (those
that do not cause symptoms). However, professionals often use "lead
poisoning" and "lead toxicity" interchangeably, and official
sources do not always restrict the use of "lead poisoning" to refer
only to symptomatic effects of lead.
The amount of
lead in the blood and tissues, as well as the time course of exposure,
determine toxicity. Lead poisoning may be acute (from intense
exposure of short duration) or chronic (from repeat low-level exposure over a
prolonged period), but the latter is much more common.[20] Diagnosis
and treatment of lead exposure are based on blood lead level (the amount of
lead in the blood), measured in micrograms of lead
per deciliter of blood
(μg/dL). Urine lead levels may be used as well, though less commonly. In cases
of chronic exposure, lead often sequesters in the highest concentrations first
in the bones, then in the kidneys. If a provider is performing a provocative
excretion test, or "chelation challenge", a measurement obtained from
urine rather than blood is likely to provide a more accurate representation of
total lead burden to a skilled interpreter.
The US Centers for Disease Control and Prevention and
the World Health Organization state that
a blood lead level of 10 μg/dL or above is a cause for concern; however,
lead may impair development and have harmful health effects even at lower
levels, and there is no known safe exposure level. Authorities such as the
American Academy of Pediatrics define lead poisoning as blood lead levels
higher than 10 μg/dL.
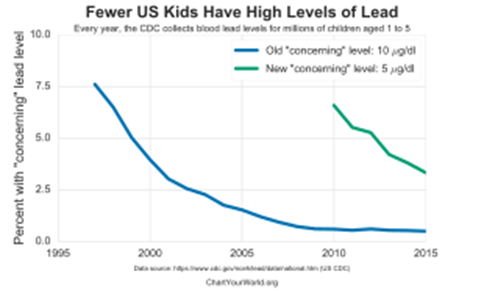
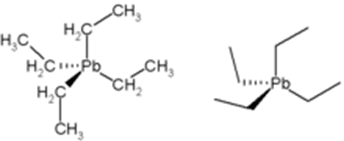
Lead forms a
variety of compounds and exists in the environment in various forms. Features
of poisoning differ depending on whether the agent is an organic compound (one that
contains carbon), or an inorganic one.[26] Organic
lead poisoning is now very rare, because countries across the world have phased
out the use of organic lead compounds as gasoline
additives, but such compounds are still
used in industrial settings. Organic lead compounds, which cross the skin
and respiratory tract easily, affect the central nervous system predominantly.
Signs and symptoms
Symptoms of lead poisoning
Lead poisoning
can cause a variety of symptoms and signs which vary
depending on the individual and the duration of lead exposure. Symptoms are nonspecific and may be subtle,
and someone with elevated lead levels may have no symptoms. Symptoms usually develop
over weeks to months as lead builds up in the body during a chronic exposure, but
acute symptoms from brief, intense exposures also occur. Symptoms from exposure to
organic lead, which is more toxic than inorganic lead due to its lipid
solubility, occur rapidly. Poisoning by organic lead compounds has
symptoms predominantly in the central nervous system, such as insomnia, delirium, cognitive deficits, tremor, hallucinations,
and convulsions.
Symptoms may be
different in adults and children; the main symptoms in adults are
headache, abdominal pain, memory loss, kidney failure, male
reproductive problems, and weakness, pain, or tingling in the extremities.
Early symptoms of
lead poisoning in adults are commonly nonspecific and include depression, loss
of appetite, intermittent abdominal pain, nausea, diarrhea, constipation,
and muscle pain. Other early signs in adults include malaise, fatigue,
decreased libido, and problems
with sleep. An unusual taste in the mouth and personality
changes are also early signs.
In adults,
symptoms can occur at levels above 40 mg./dL, but are more likely to occur
only above 50–60 go/dL. Symptoms begin to appear in children generally
at around 60 mg./dL. However,
the lead levels at which symptoms appear vary widely depending on unknown
characteristics of each individual. At blood lead levels between 25 and 60 go/dL, neuropsychiatric effects
such as delayed reaction times, irritability,
and difficulty concentrating, as well as slowed motor nerve conduction
and headache can occur. Anemia may appear
at blood lead levels higher than 50 mg./dL. In adults,
abdominal colic, involving paroxysms of pain,
may appear at blood lead levels greater than 80 go/dL. Signs that
occur in adults at blood lead levels exceeding 100 mg./dL include wrist drop and foot drop, and signs
of encephalopathy (a
condition characterized by brain
swelling), such as those that accompany
increased pressure within the skull, delirium,
coma, seizures, and headache. In
children, signs of encephalopathy such as bizarre behavior, discoordination,
and apathy occur at lead levels exceeding 70 go/dL For both adults
and children, it is rare to be asymptomatic if blood lead levels exceed
100 mg./dL.
Acute poisoning
In acute
poisoning, typical neurological signs are pain, muscle weakness, numbness and tingling, and, rarely,
symptoms associated with inflammation of the brain. Abdominal
pain, nausea, vomiting, diarrhea, and constipation are other acute symptoms. Lead's effects on the mouth
include astringency and a
metallic taste. Gastrointestinal problems, such as constipation, diarrhea, poor appetite, or weight loss, are common in
acute poisoning. Absorption of large amounts of lead over a short time can
cause shock (insufficient fluid in
the circulatory
system) due to loss of water from the
gastrointestinal tract. ] Hemolysis (the
rupture of red blood cells) due to acute
poisoning can cause anemia and hemoglobin in the urine. Damage to kidneys can
cause changes in urination such as acquired fanconi syndrome and decreased urine output. People
who survive acute poisoning often go on to display symptoms of chronic
poisoning.
Chronic poisoning
Chronic poisoning
usually presents with symptoms affecting multiple systems, but is
associated with three main types of symptoms: gastrointestinal, neuromuscular, and neurological. Central nervous system and
neuromuscular symptoms usually result from intense exposure, while
gastrointestinal symptoms usually result from exposure over longer periods. Signs of chronic exposure
include loss of short-term memory or
concentration, depression, nausea, abdominal pain, loss of coordination, and
numbness and tingling in the extremities. Fatigue, problems with sleep,
headaches, stupor, slurred speech, and anemia are also found in chronic lead
poisoning. A
"lead hue" of the skin with pallor and/or lividity is another
feature. A blue line
along the gum with bluish black edging to the teeth, known as a Burton line, is another
indication of chronic lead poisoning. Children with chronic
poisoning may refuse to play or may have hyperkinetic or aggressive behavior
disorders. Visual
disturbance may present with gradually progressing blurred vision as a result
of central scotoma, caused by
toxic optic neuritis.
Effects on /children
A pregnant woman
who has elevated blood lead levels is at greater risk of a premature birth or
with a low birth weight. Children
are more at risk for lead poisoning because their smaller bodies are in a
continuous state of growth and development. Young
children are much more vulnerable to lead poisoning, as they absorb 4 to 5
times more lead than an adult from a given source. Furthermore,
children, especially as they are learning to crawl and walk, are constantly on
the floor and therefore more prone to ingesting and inhaling dust that is
contaminated with lead.
The classic signs
and symptoms in children are loss of appetite, abdominal pain, vomiting, weight
loss, constipation, anemia, kidney failure, irritability, lethargy, learning
disabilities, and behavioral problems. Slow
development of normal childhood behaviors, such as talking and use of words,
and permanent intellectual disability are both
commonly seen. Although less common, it is possible for fingernails to
develop leukonychia striata if exposed
to abnormally high lead concentrations.
On July 30, 2020,
a report by UNICEF and Pure Earth revealed
that lead poisoning is affecting children on a "massive and previously
unknown scale". According to the report, one in three children, up to 800
million globally, have blood lead levels at, or above, 5 micrograms per
decilitre (µg/dL), the amount at which action is required.
By organ system
Lead affects
every one of the body's organ systems, especially the nervous system, but also
the bones and teeth, the kidneys, and the cardiovascular, immune, and reproductive systems. Hearing loss and tooth decay have been
linked to lead exposure, as have cataracts. Intrauterine and neonatal
lead exposure promote tooth decay. Aside from the developmental
effects unique to young children, the health effects experienced by adults are
similar to those in children, although the thresholds are generally higher.
Kidneys
Kidney damage
occurs with exposure to high levels of lead, and evidence suggests that lower
levels can damage kidneys as well. The toxic effect of lead
causes nephropathy and may
cause Fanconi syndrome, in which the proximal tubular function of
the kidney is impaired. Long-term
exposure at levels lower than those that cause lead nephropathy have also been
reported as nephrotoxic in patients
from developed countries that had chronic kidney disease or were at risk
because of hypertension or diabetes
mellitus. Lead poisoning inhibits
excretion of the waste product urate and causes
a predisposition for gout, in which urate
builds up. This condition is known
as saturnine gout.
Cardiovascular system
Evidence suggests
lead exposure is associated with high blood pressure, and studies
have also found connections between lead exposure and coronary heart disease, heart rate variability, and death from
stroke, but this evidence is more limited. People who have been exposed to higher
concentrations of lead may be at a higher risk for cardiac autonomic dysfunction on days
when ozone and fine
particles are higher.
Reproductive system
Lead affects both
the male and female reproductive systems. In men, when blood lead levels exceed
40 μg/dL, sperm count is reduced
and changes occur in volume of sperm, their motility, and their morphology.
A pregnant woman's elevated blood lead level can
lead to miscarriage, prematurity, low birth weight, and problems
with development during childhood. Lead is able to pass through
the placenta and into
breast milk, and blood lead levels in mothers and infants are usually similar. A fetus may be poisoned in utero if
lead from the mother's bones is subsequently mobilized by the changes in
metabolism due to pregnancy; increased calcium intake in pregnancy may help
mitigate this phenomenon.
Nervous system
The brains of
adults who were exposed to lead as children show decreased volume, especially in the prefrontal cortex, on MRI. Areas of volume loss are shown in color over a template of a normal brain.
Lead affects
the peripheral nervous system (especially motor nerves) and the central nervous system. Peripheral nervous system
effects are more prominent in adults and central nervous system effects are
more prominent in children. Lead causes
the axons of nerve cells to
degenerate and lose their myelin coats.
Lead exposure in
young children has been linked to learning disabilities, and
children with blood lead concentrations greater than 10 μg/dL are in
danger of developmental disabilities. Increased
blood lead level in children has been correlated with decreases in intelligence, nonverbal reasoning, short-term memory, attention,
reading and arithmetic ability, fine motor skills, emotional regulation, and social engagement.
The effect of
lead on children's cognitive abilities takes place at very low levels. There
is apparently no lower threshold to the dose-response relationship (unlike
other heavy metals such as mercury). Reduced
academic performance has been associated with lead exposure even at blood lead
levels lower than 5 μg/dL. Blood lead
levels below 10 μg/dL have been reported to be associated with lower IQ
and behavior problems such as aggression, in proportion with blood lead levels. Between the blood lead
levels of 5 and 35 μg/dL, an IQ decrease of 2–4 points for each μg/dL
increase is reported in children. However, studies that show associations
between low-level lead exposure and health effects in children may be affected
by confounding and
overestimate the effects of low-level lead exposure.
High blood lead
levels in adults are also associated with decreases in cognitive performance
and with psychiatric symptoms such as depression and anxiety. It was
found in a large group of current and former inorganic lead workers in Korea
that blood lead levels in the range of 20–50 μg/dL were correlated with
neuro-cognitive defects. Increases in blood lead levels from about 50 to
about 100 μg/dL in adults have been found to be associated with
persistent, and possibly permanent, impairment of central nervous system
function.
Lead exposure in
children is also correlated with neuropsychiatric disorders such as attention deficit hyperactivity disorder and anti-social behaviour. Elevated
lead levels in children are correlated with higher scores on aggression and
delinquency measures. A
correlation has also been found between prenatal and early childhood lead
exposure and violent crime in adulthood. Countries
with the highest air lead levels have also been found to have the highest
murder rates, after adjusting for confounding factors. A May 2000 study by economic
consultant Rick Nevin theorizes
that lead exposure explains 65% to 90% of the variation in violent crime rates
in the US. A 2007
paperme author claims to show a strong association between preschool blood lead
and subsequent crime rate trends over several decades across nine countries. Lead
exposure in childhood appears to increase school suspensions and juvenile
detention among boys It is
believed that the U.S. ban on lead paint in buildings in the late 1970s, as
well as the phaseout of leaded gasoline in the 1970s and 1980s, partially
helped contribute to the decline of violent crime in the United States since
the early 1990s.
Lead is a common environmental
pollutant. Causes of
environmental contamination include industrial use of lead, such as found in
facilities that process lead-acid batteries or produce lead wire or pipes, and
metal recycling and foundries. Storage
batteries and ammunition are made with the largest amounts of lead consumed in
the economy each year, in the US as of 2013. Children
living near facilities that process lead, such as lead smelters, have been found
to have unusually high blood lead levels. In August 2009, parents
rioted in China after lead poisoning was found in nearly 2000 children living near
zinc and manganese smelters. Lead exposure can
occur from contact with lead in air, household dust, soil, water, and
commercial products. Leaded gasoline has also
been linked to increases in lead pollution. Some research has suggested a
link between leaded gasoline and crime rates
Man made lead pollution has been elevated in the air for the past
2000 years. Lead pollution in the
air is entirely due to human activity (mining and smelting, as well as in
gasoline).
Occupational exposure
Battery
recycling workers are at risk for lead
exposure. This worker
ladles molten lead into billets in a lead-acid battery recovery facility.
In adults, occupational exposure is the main cause of
lead poisoning. People can be exposed when working in facilities that
produce a variety of lead-containing products; these include radiation
shields, ammunition, certain surgical
equipment, developing dental X-ray films prior to digital X-rays (each film
packet had a lead liner to prevent the radiation from going through), fetal
monitors, plumbing, circuit boards, jet engines, and ceramic glaze. In addition, lead miners and smelters,
plumbers and fitters, auto mechanics, glass manufacturers, construction
workers, battery manufacturers and recyclers, firing range workers,
and plastic manufacturers are at risk for lead exposure. Other occupations
that present lead exposure risks include welding, manufacture of rubber,
printing, zinc and copper smelting,
processing of ore, combustion
of solid waste, and production
of paints and pigments. Lead exposure can also occur
with intense use of gun ranges, regardless of
whether these ranges are indoor or out. Parents
who are exposed to lead in the workplace can bring lead dust home on clothes or
skin and expose their children/ Occupational exposure to lead increases
the risk of cardiovascular disease, in
particular: stroke, and high blood pressure.
Food
Lead may be found
in food when food is grown in soil that is high in lead, airborne lead
contaminates the crops, animals eat lead in their diet, or lead enters the food
either from what it was stored or cooked in. Ingestion
of lead paint and batteries is also a route of exposure for livestock, which
can subsequently affect humans. Milk produced by contaminated cattle can be
diluted to a lower lead concentration and sold for consumption.
In Bangladesh,
lead compounds have been added to turmeric to make it more yellow This is believed to have started in
the 1980s and continues as of 2019. It is
believed to be one of the main sources of high lead levels in the
country. In Hong Kong the maximum allowed lead parts per million is 6 in solid
foods and 1 in liquid foods.
Paint
Some lead
compounds are colorful and are used widely in paints, and lead paint is a major route of lead
exposure in children. A study conducted in 1998–2000
found that 38 million housing units in the US had lead-based paint, down from a
1990 estimate of 64 million. Deteriorating lead paint can produce dangerous
lead levels in household dust and soil. Deteriorating
lead paint and lead-containing household dust are the main causes of chronic
lead poisoning. The lead
breaks down into the dust and since children are more prone to crawling on the
floor, it is easily ingested. Many young
children display pica, eating things
that are not food. Even a small amount of a lead-containing product such as a
paint chip or a sip of glaze can contain tens or hundreds of milligrams of
lead. Eating
chips of lead paint presents a particular hazard to children, generally
producing more severe poisoning than occurs from dust.
Because removing lead paint from dwellings, e.g. by
sanding or torching, creates lead-containing dust and fumes, it is generally
safer to seal the lead paint under new paint (excepting moveable windows and
doors, which create paint dust when operated. Alternatively, special precautions must be
taken if the lead paint is to be removed.
In oil painting, it was once
common for colors such as yellow or white to be made with lead carbonate. Lead white oil color
was the main white of oil painters until superseded by compounds
containing zinc or titanium in the
mid-20th century. It is speculated that the painter Caravaggio and
possibly Francisco Goya and Vincent Van Gogh had lead poisoning due to
overexposure or carelessness when handling this color.
Soil
\\\\
A lead warning on a fuel pump. Tetraethyllead, which used to
be added to automotive gasoline (and still is added to some aviation gasolines), contributed
to soil contamination.
Residual lead in
soil contributes to lead exposure in urban areas. It has been
thought that the more polluted an area is with various contaminants, the more
likely it is to contain lead. However, this is not always the case, as there
are several other reasons for lead contamination in soil.
Lead content in
soil may be caused by broken-down lead paint, residues from lead-containing
gasoline, used engine oil, tire weights, or pesticides used in the
past, contaminated landfills, or from nearby industries such as foundries or smelters
For example, in the Montevideo neighborhood
of LaTeja, former
industrial sites became important sources of exposure in local communities in
the early 2000s. Although leaded soil is less of a problem in countries
that no longer have leaded gasoline, it remains
prevalent, raising concerns about the safety of urban agriculture; eating
food grown in contaminated soil can present a lead hazard. Interfacial
solar eva.
Transportation
has been recently studied as a technique for remediating lead-contaminated
sites, which involves the evaporation of heavy metal ions from moist soil.
Water
Lead from the
atmosphere or soil can end up in groundwater and surface water. It is also potentially
in drinking water, e.g. from
plumbing and fixtures that are either made of lead or have lead solder. Since acidic water breaks down
lead in plumbing more readily, chemicals can be added to municipal water to
increase the pH and thus
reduce the corrosivity of the
public water supply. Chloramines, which were
adopted as a substitute for chlorine disinfectants due to
fewer health concerns, increase corrositivity. In the US, 14–20% of total
lead exposure is attributed to drinking water. In 2004, a
team of seven reporters from The Washington Post discovered high levels of lead in the drinking water in Washington, DC, and won an award
for investigative reporting for a
series of articles about this contamination. In the water crisis
in Flint, Michigan, a switch to a more corrosive
municipal water source caused elevated lead levels in domestic tap water.
Like Flint MI and Washington DC, a similar situation affects the State of Wisconsin, where estimates call for replacement of up to 176,000.
0 underground
pipes made of lead known as lead service lines. The city
of Madison,
Wisconsin addressed the issue and
replaced all of their lead service lines, but there are still others that have
yet to follow suit. While there are chemical methods that could help reduce the
amount of lead in the water distributed, a permanent fix would be to replace
the pipes completely. While the state may replace the pipes below ground, it
will be up to the homeowners to replace the pipes on their property, at an
average cost of $3,000. Experts say
that if the city were to replace their pipes and the citizens were to keep the
old pipes located within their homes, there would be a potential for more lead
to dissolve into their drinking water. The U.S. Congress authorized the
EPA to dedicate funds to assist states and nonprofits with the costs of lead
service line removal under Section 50105 of the Safe Drinking Water Act.
Collected rainwater from roof runoff used as potable water may contain lead, if there are lead contaminants on the roof or in the storage tank.[22] The Australian Drinking Water Guidelines allow a maximum of 0.01 mg/L (10 ppb) lead in water.
Lead wheel
weights have been found to accumulate on roads and interstates and erode in
traffic entering the water runoff through drains. Leaded fishing weights
accumulate in rivers, streams, ponds, and lakes.
Gasoline
Tetraethyllead was first
added to gasoline in 1923, as it helped prevent engine knocking. Automotive
exhaust represented a major way for lead to be inhaled, invade the bloodstream
and pass into the brain.
The use of lead
in gasoline peaked in the 1970s. By the next decade most high incomes countries
prohibited the use of leaded petrol. As late as 2002, almost all low-and
middle-income countries including some OECD members still used it. The UN
Environment Program (UNEP) thus launched a campaign in 2002 to eliminate its
use, leading to Algeria being the last country to stop its use in July 2021.
Lead-containing products
Lead can be found
in products such as kohl, an ancient
cosmetic from the Middle East, South Asia, and parts of Africa that has many
other names; and from some toys. In 2007, millions of toys made in China were recalled from
multiple countries owing to safety hazards including lead paint. Vinyl mini-blinds, found
especially in older housing, may contain lead. Lead is commonly
incorporated into herbal remedies such as
Indian Ayurvedic preparations
and remedies of Chinese origin. There are
also risks of elevated blood lead levels caused by folk remedies like azarcon and greta,
which each contain about 95% lead.
Ingestion of
metallic lead, such as small lead fishing lures, increases blood lead levels
and can be fatal. Ingestion
of lead-contaminated food is also a threat. Ceramic glaze often contains lead,
and dishes that have been improperly fired can leach the metal into food,
potentially causing severe poisoning. In
some places, the solder in cans used for food contains lead.[34] When
manufacturing medical instruments and hardware, solder containing lead may be
present. People who
eat animals hunted with lead bullets may be at risk for lead exposure. Bullets lodged in the human
body rarely cause significant levels of lead, but bullets lodged in the
joints are the exception, as they deteriorate and release lead into the body
over time.
In May 2015,
Indian food safety regulators in the state of Uttar Pradesh found that samples
of Maggi 2 Minute
Noodles contained lead up to 17
times beyond permissible limits. On 3 June
2015, New Delhi Government
banned the sale of Maggi noodles in New Delhi stores for 15 days because it was
found to contain lead beyond the permissible limit. The Gujarat FDA on 4
June 2015 banned the noodles for 30 days after 27 out of 39 samples were
detected with objectionable levels of metallic lead, among other things. Some of India's biggest
retailers like Future Group, Big Bazaar, Easyday and
Nilgiris have imposed a nationwide ban on Maggi noodles. Many other
states too have banned Maggi noodles.
Bullets
Contact with ammunition is a source of lead exposure. As
of 2013, lead-based ammunition production is the second largest annual use of
lead in the US, accounting for over 84,800 metric tons consumed in
2013, second only to the manufacture of storage batteries. The
Environmental Protection Agency (EPA) cannot regulate cartridges and shells, as
a matter of law. Lead birdshot is banned
in some areas, but this is primarily for the benefit of the birds and their
predators, rather than humans. Contamination
from heavily used gun ranges is of concern to those who live near by. Non-lead alternatives
include copper, zinc, steel, tungsten-nickel-iron, bismuth-tin, and polymer
blends such as tungsten-polymer and copper-polymer.
Because game animals can be shot using lead bullets, the
potential for lead ingestion from game meat consumption has been studied
clinically and epidemiologically. In a recent study conducted by the CDC, a cohort from North Dakota was enrolled and
asked to self-report historical consumption of game meat, and participation in
other activities that could cause lead exposure. The study found that
participants' age, sex, housing age, current hobbies with potential for lead
exposure, and game consumption were all associated with blood lead level (PbB).
According to a study published in 2008, 1.1% of the 736
persons consuming wild game meat tested had PbB ≥5 μg/dl. In November 2015 The US
HHS/CDC/NIOSH designated 5 µg/dL (five micrograms per deciliter) of whole
blood, in a venous blood sample, as the reference blood lead level for adults.
An elevated BLL is defined as a BLL ≥5 µg/dL. This case definition is used
by the ABLES program, the Council of State and Territorial Epidemiologists (CSTE),
and CDC's National Notifiable Diseases Surveillance System (NNDSS). Previously
(i.e. from 2009 until November 2015), the case definition for an elevated BLL
was a BLL ≥10 µg/dL.
Jacketed ammunition (left), bare
lead (right)
To virtually eliminate
the potential for lead contamination, some researchers have suggested the use
of lead-free copper non-fragmenting bullets.
Bismuth is an
element used as a lead-replacement for shotgun pellets used in waterfowl
hunting although shotshells made from bismuth are nearly ten times the cost of
lead.
Opium
Lead
contaminated opium has been
the source of poisoning in Iran and other Middle Eastern countries. This has
also appeared in the illicit narcotic supply in North America, resulting in
confirmed lead poisoning.
Pathophysiology
Tetraethyllead, still used as
an additive in some fuels, can be absorbed through the skin.
Exposure occurs
through inhalation, ingestion or
occasionally skin contact. Lead may be
taken in through direct contact with mouth, nose, and eyes (mucous membranes),
and through breaks in the skin. Tetraethyllead, which was a
gasoline additive and is still used in aviation gasoline, passes through
the skin; and other forms of lead, including inorganic lead. are also
absorbed through skin. The main sources of absorption of inorganic lead are
from ingestion and inhalation. In adults,
about 35–40% of inhaled lead dust is deposited in the lungs, and about 95% of
that goes into the bloodstream. Of ingested
inorganic lead, about 15% is absorbed, but this percentage is higher in
children, pregnant women, and people with deficiencies of calcium, zinc, or
iron. Infants may absorb about 50% of ingested lead, but little is known
about absorption rates in children.
The main body
tissues that store lead are the blood, soft tissues, and bone; the half-life of
lead in these tissues is measured in weeks for blood, months for soft tissues,
and years for bone. Lead in the bones, teeth, hair, and nails is bound
tightly and not available to other tissues and is generally thought not to be
harmful. In adults,
94% of absorbed lead is deposited in the bones and teeth, but children only
store 70% in this manner, a fact which may partially account for the more serious
health effects on children. The half-life of lead in bone has been
estimated as years to decades, and bone can introduce lead into the bloodstream
long after the initial exposure is gone. The half-life of lead in the
blood in men is about 40 days, but it may be longer in children and pregnant
women, whose bones are undergoing remodeling, which allows
the lead to be continuously re-introduced into the bloodstream. Also, if
lead exposure takes place over years, clearance is much slower, partly due to
the re-release of lead from bone. Many other tissues store lead, but those
with the highest concentrations (other than blood, bone, and teeth) are the
brain, spleen, kidneys, liver, and lungs. Lead is removed from the body
very slowly, mainly through urine. Smaller amounts of lead are also
eliminated through the feces, and very small amounts in hair, nails, and sweat.
Lead has no known
physiologically relevant role in the body and its harmful effects are
myriad. Lead and other heavy metals create reactive radicals which
damage cell structures including DNA and cell membranes. Lead also
interferes with DNA transcription, enzymes that help
in the synthesis of vitamin D, and enzymes
that maintain the integrity of the cell
membrane., insomnia may result when the cell membranes
of red blood cells become more
fragile as the result of damage to their membranes. Lead interferes with
metabolism of bones and teeth and alters the permeability of blood vessels
and collagen synthesis. ]Lead may also be
harmful to the developing immune
system, causing production of
excessive inflammatory proteins;
this mechanism may mean that lead exposure is a risk factor for asthma in
children. Exposure
has also been associated with a decrease in activity of immune cells such
as polymorphonuclear leukocytes/ Lead also
interferes with the normal metabolism of calcium in
cells and causes it to build up within them.
Enzymes
ALAD enzyme with lead
bound (PDB: 1QNV)
The primary cause
of lead's toxicity is its interference with a variety of enzymes because it
binds to sulfhydryl groups found on
many enzymes. Part of
lead's toxicity results from its ability to mimic other metals that take part
in biological processes, which act as cofactors in many enzymatic reactions,
displacing them at the enzymes on which they act. Lead is able to bind to
and interact with many of the same enzymes as these
metals but, due to its differing chemistry, does not properly function as a
cofactor, thus interfering with the enzyme's ability to catalyze its normal
reaction or reactions. Among the essential metals with which lead interacts are
calcium, iron, and zinc.
The lead ion has
a lone pair in its
electronic structure, which can result in a distortion in the coordination of ligands, and in 2007 was
hypothesized to be important in lead poisoning's effects on enzymes (see Lone pair § Unusual lone
pairs).
One of the main
causes for the pathology of lead is that it interferes with the activity of an essential
enzyme called delta-aminolevulinic
acid dehydratase, or ALAD (see image of the enzyme
structure), which is important in the biosynthesis of heme, the cofactor
found in hemoglobin. Lead also
inhibits the enzyme ferrochelatase, another enzyme involved in the
formation of heme. Ferrochelatase
catalyzes the joining of protoporphyrin and Fe2+ to form
heme. Lead's
interference with heme synthesis results in production of zinc protoporphyrin and the
development of anemia. Another effect
of lead's interference with heme synthesis is the buildup of heme precursors,
such as aminolevulinic acid, which may be
directly or indirectly harmful to neurons. Elevation of aminolevulinic acid
results in lead poisoning having symptoms similar to acute porphyria.
Neurons
Lead exposure damages cells in the hippocampus, a part of the brain involved in memory. Hippocampi of lead-exposed rats (bottom) show structural damage such as irregular nuclei (IN) and denaturation of myelin (DMS) compared to controls (top).
The brain is the organ most sensitive to lead exposure. Lead is able to pass through the endothelial cells at the blood brain barrier because it can substitute for calcium ions and be taken up by calcium-ATPase pumps. Lead poisoning interferes with the normal development of a child's brain and nervous system; therefore children are at greater risk of lead neurotoxicity than adults are. In a child's developing brain, lead interferes with synapse formation in the cerebral cortex, neurochemical development (including that of neurotransmitters), and organization of ion channels. It causes loss of neurons' myelin sheaths, reduces numbers of neurons, interferes with neurotransmission, and decreases neuronal growth.
Lead-ions (Pb2+),
like magnesium-ions (Mg2+), block NMDA receptors. Therefore, an
increase in Pb2+ concentration will effectively inhibit
ongoing long-term potentiation (LTP), and
lead to an abnormal increase in long-term depression (LTD)
on neurons in the
affected parts of the nervous system. These
abnormalities lead to the indirect downregulation of NMDA-receptors,
effectively initiating a positive
feedback-loop for LTD. The targeting of NMDA receptors is thought to
be one of the main causes for lead's toxicity to neurons.
Diagnosis
includes determining the clinical signs and the medical history, with inquiry
into possible routes of exposure. Clinical
toxicologists, medical specialists in the area
of poisoning, may be involved in diagnosis and treatment. The main tool in diagnosing
and assessing the severity of lead poisoning is laboratory analysis of
the blood lead level (BLL).
Basophilic stippling (arrows) of
red blood cells in a
53-year-old who had elevated blood lead levels due to drinking repeatedly from
glasses decorated with lead paint.
Blood film examination
may reveal basophilic stippling of
red blood cells (dots in
red blood cells visible through a microscope), as well as the changes normally
associated with iron-deficiency anemia (microcytosis and hypochromasia). This may be
known as sideroblastic anemia However, basophilic stippling is also
seen in unrelated conditions, such as megaloblastic anemia caused by vitamin B12
(colbalamin) and folate deficiencies. Contrary to
other sideroblastic anemia, there are no ring sideroblasts in a bone marrow
smear.
Exposure to lead
also can be evaluated by measuring erythrocyte protoporphyrin (EP) in
blood samples. EP is a
part of red blood cells known to increase when the amount of lead in the blood
is high, with a delay of a few weeks. Thus EP levels in conjunction
with blood lead levels can suggest the time period of exposure; if blood lead
levels are high but EP is still normal, this finding suggests exposure was
recent. However,
the EP level alone is not sensitive enough to identify elevated blood lead
levels below about 35 μg/dL. Due to this higher threshold for
detection and the fact that EP levels also increase in iron deficiency, use of this method for detecting
lead exposure has decreased.
Blood levels are an indicator mainly of recent or
current lead exposure, not of total body burden. Lead in
bones can be measured noninvasively by X-ray
fluorescence; this may be the best measure of
cumulative exposure and total body burden. However
this method is not widely available and is mainly used for research rather than
routine diagnosis. Another
radiographic sign of elevated lead levels is the presence of radiodense lines
called lead lines at the metaphysis in the long
bones of growing children, especially around the knees.
These
lead lines, caused by increased calcification due to
disrupted metabolism in the growing bones, become wider as the duration of lead
exposure increases.[196] X-rays may also
reveal lead-containing foreign materials such as paint chips in the
gastrointestinal tract.
Fecal lead
content that is measured over the course of a few days may also be an accurate
way to estimate the overall amount of childhood lead intake. This form of
measurement may serve as a useful way to see the extent of oral lead exposure
from all the diet and environmental sources of lead.
Lead poisoning
shares symptoms with other conditions and may be easily missed. Conditions that present
similarly and must be ruled out in diagnosing lead poisoning include .
Guillain–Barré syndrome, renal colic, appendicitis, encephalitis in adults,
and viral gastroenteritis in
children. Other differential diagnoses in children
include constipation, abdominal
colic, iron deficiency, subdural
hematoma, neoplasms of the
central nervous system, emotional and behavior disorders, and intellectual disability.
Reference levels
The current
reference range for acceptable blood lead concentrations in healthy persons
without excessive exposure to environmental sources of lead is less than
3.5 µg/dL for children. It was less than
25 µg/dL for adults. Previous to
2012 the value for children was 10 (µg/dl). Lead-exposed workers in the
U.S. are required to be removed from work when their level is greater than
50 µg/dL if they do construction and otherwise greater than 60 µg/dL.
In 2015, US
HHS/CDC/NIOSH designated 5 µg/dL (five micrograms per deciliter) of whole
blood, in a venous blood sample, as the reference blood lead level for adults.
An elevated BLL is defined as a BLL ≥5 µg/dL. This case definition is used
by the ABLES program, the Council of State and Territorial Epidemiologists
(CSTE), and CDC's National Notifiable Diseases Surveillance System (NNDSS).
Previously (i.e. from 2009 until November 2015), the case definition for an
elevated BLL was a BLL ≥10 µg/dL. The U.S. national
BLL geometric mean among adults was 1.2 μg/dL in 2009–2010.
Blood lead
concentrations in poisoning victims have ranged from 30 to 80 µg/dL in
children exposed to lead paint in older houses, 77–104 µg/dL in persons
working with pottery glazes, 90–137 µg/dL in individuals consuming
contaminated herbal medicines, 109–139 µg/dL in indoor shooting range
instructors and as high as 330 µg/dL in those drinking fruit juices from
glazed earthenware containers.
\
Testing kits are commercially
available for detecting lead. These swabs, when wiped on a surface, turn red in
the presence of lead.
In most cases,
lead poisoning is preventable by avoiding exposure to lead. Prevention
strategies can be divided into individual (measures taken by a family),
preventive medicine (identifying and intervening with high-risk individuals),
and public health (reducing risk on a population level).
Recommended steps
by individuals to reduce the blood lead levels of children include increasing
their frequency of hand washing and their intake of calcium and iron,
discouraging them from putting their hands to their mouths, vacuuming
frequently, and eliminating the presence of lead-containing objects such as
blinds and jewellery in the house. In houses
with lead pipes or plumbing solder, these can be replaced. Less permanent
but cheaper methods include running water in the morning to flush out the most
contaminated water or adjusting the water's chemistry to prevent corrosion of
pipes. Lead
testing kits are commercially available for detecting the presence of lead in
the household. Testing kit accuracy depends on the user testing all layers
of paint and the quality of the kit; the US Environmental Protection Agency (EPA) only
approves kits with an accuracy rating of at least 95%. Professional lead
testing companies caution that DIY test kits can create health risks for users
that do not understand their limitations and liability issues for employers
with regard to worker protection. As hot
water is more likely than cold water to contain higher amounts of lead, use
only cold water from the tap for drinking, cooking, and making baby formula.
Since most of the lead in household water usually comes from plumbing i
n the house and
not from the local water supply, using cold water can avoid lead exposure. Measures such as dust control and household
education do not appear to be effective in changing children's blood levels.
Prevention
measures also exist on national and municipal levels. Recommendations by health
professionals for lowering childhood exposures include banning the use of lead
where it is not essential and strengthening regulations that limit the amount
of lead in soil, water, air, household dust, and products. Regulations
exist to limit the amount of lead in paint; for example, a 1978 law in the US
restricted the lead in paint for residences, furniture, and toys to 0.06% or
less.[110] In October
2008, the US EPA reduced the allowable lead level by a factor of ten to 0.15
micrograms per cubic meter of air, giving states five years to comply with the
standards. The
European Union's Restriction of Hazardous Substances Directive limits
amounts of lead and other toxic substances in electronics and electrical
equipment. In some places, remediation programs exist to reduce the presence of
lead when it is found to be high, for example in drinking water. As a more
radical solution, entire towns located near former lead mines have been
"closed" by the government, and the population resettled elsewhere,
as was the case with Picher,
Oklahoma, in 2009.
Screening
Screening may be
an important method of prevention for those at high risk such as those who
live near lead-related industries. The USPSTF
has stated that general screening of those without symptoms include children
and pregnant women is of unclear benefit as of 2019. The ACOG and APP,
however, recommends asking about risk factors and testing those who have them.
Education
The education of
workers on lead, its danger and how its workplace exposure can be decreased,
especially when initial blood lead level and urine lead level are high, could
help reduce the risk of lead poisoning in the workplace.
The mainstays of
treatment are removal from the source of lead and, for people who have
significantly high blood lead levels or who have symptoms of poisoning, chelation
therapy. Treatment
of iron, calcium, and zinc deficiencies, which are
associated with increased lead absorption, is another part of treatment for
lead poisoning. When lead-containing materials are present in
the gastrointestinal tract (as evidenced by abdominal X-rays), whole bowel irrigation, cathartics, endoscopy, or even
surgical removal may be used to eliminate it from the gut and prevent further
exposure. Lead-containing
bullets and shrapnel may also present a threat of further exposure and may need
to be surgically removed if they are in or near fluid-filled or synovial spaces. If
lead encephalopathy is present, anticonvulsants may be
given to control seizures, and treatments to control swelling of the brain include corticosteroids and mannitol. Treatment
of organic lead poisoning involves removing the lead compound from the skin,
preventing further exposure, treating seizures, and possibly chelation therapy
for people with high blood lead concentrations.
Before the advent of organic chelating
agents, salts of iodide were given
orally, such as heavily popularized by Louis Melsens and many
nineteenth and early twentieth century doctors.
A chelating agent
is a molecule with at least two negatively charged groups that allow it to form
complexes with metal ions with multiple positive charges, such as lead. The chelate that is
thus formed is nontoxic and can be excreted in the urine, initially at up
to 50 times the normal rate. The chelating agents used for treatment of
lead poisoning are edetate disodium calcium (CaNa2EDTA), dimercaprol (BAL),
which are injected, and succimer and d-penicillamine, which are
administered orally. Chelation
therapy is used in cases of acute
lead poisoning, severe poisoning, and encephalopathy, and is
considered for people with blood lead levels above 25 µg/dL. While the
use of chelation for people with symptoms of lead poisoning is widely
supported, use in asymptomatic people with high blood lead levels is more
controversial. Chelation
therapy is of limited value for cases of chronic exposure to low levels of
lead. Chelation therapy is usually stopped when symptoms resolve or when
blood lead levels return to premorbid levels. When lead exposure has taken
place over a long period, blood lead levels may rise after chelation is stopped
because lead is leached into blood from stores in the bone; thus
repeated treatments are often necessary.
People receiving
dimercaprol need to be assessed for peanut allergies since the commercial formulation
contains peanut oil. Calcium EDTA is also effective if administered four hours
after the administration of dimercaprol. Administering dimercaprol, DMSA
(Succimer), or DMPS prior to
calcium EDTA is necessary to prevent the redistribution of lead into the
central nervous system. Dimercaprol used alone may
also redistribute lead to the brain and testes.
An adverse side effect of calcium EDTA is renal
toxicity. Succimer (DMSA) is the preferred agent in mild to moderate lead
poisoning cases. This may be the case in instances where children have a blood
lead level >25μg/dL. The most reported adverse side effect for succimer is
gastrointestinal disturbances. It is also important to note that chelation
therapy only lowers blood lead levels and may not prevent the lead-induced
cognitive problems associated with lower lead levels in tissue. This may be
because of the inability of these agents to remove sufficient amounts of lead
from tissue or inability to reverse preexisting damage.
Chelating agents can have adverse effects; for
example, chelation therapy can lower the body's levels of necessary nutrients
like zinc.[ Chelating
agents taken orally can increase the body's absorption of lead through the
intestine.
Chelation
challenge, also known as provocation testing, is used to indicate an elevated
and mobilizable body burden of heavy metals including lead. This testing
involves collecting urine before and after administering a one-off dose of
chelating agent to mobilize heavy metals into the urine. Then urine is
analyzed by a laboratory for levels of heavy metals; from this analysis overall
body burden is inferred.[231] Chelation
challenge mainly measures the burden of lead in soft tissues, though whether it
accurately reflects long-term exposure or the amount of lead stored in bone
remains controversial. Although the technique has been used to determine
whether chelation therapy is indicated and to diagnose heavy metal exposure,
some evidence does not support these uses as blood levels after chelation are
not comparable to the reference range typically used to diagnose heavy metal
poisoning. The single chelation dose could also
redistribute the heavy metals to more sensitive areas such as central nervous
system tissue.
Since lead has
been used widely for centuries, the effects of exposure are worldwide. Environmental
lead is ubiquitous, and everyone has some measurable blood lead level. Atmospheric
lead pollution increased dramatically beginning in the 1950s as a result of the
widespread use of leaded gasoline. Lead one of the largest environmental medicine problems in
tes of numbers of people exposed and the public health toll it takes.[54] Lead
exposure accounts for about 0.2% of all deaths and 0.6% of disability adjusted life years globally.
Although
regulation reducing lead in products has greatly reduced exposure in the
developed world since the 1970s, lead is still allowed in products in many
developing countries. According to the World Health Organization, as of June
2022, only 45% of countries had confirmed legally-binding controls on
production and use of lead paint Significant
disparities exist in the enactment of bans, with regions such as the Middle East, North Africa, and Sub-Saharan
Africa currently the most likely to
have countries lacking such measures. Despite phase out in many parts of
the Global North, Global South
exposure has increased by nearly three times. In all
countries that have banned leaded gasoline, average blood lead levels have
fallen sharply. ] However, some developing
countries still allow leaded gasoline, which is the primary source of lead
exposure in most developing countries. Beyond exposure from gasoline,
the frequent use of pesticides in developing countries adds a risk of lead
exposure and subsequent poisoning. Poor children in developing
countries are at especially high risk for lead poisoning.[75] Of North
American children, 7% have blood lead lels above 10 μg/dL, whereas among
Central and South American children, the percentage is 33–34%.[204] About one
fifth of the world's disease
burden from lead poisoning occurs
in the Western Pacific, and another fifth is in Southeast Asia.
In developed
countries, people with low levels of education living in poorer areas are most
at risk for elevated lead. In the US, the groups most
at risk for lead exposure are the impoverished, city-dwellers, and immigrants. African-American children and
those living in old housing have also been found to be at elevated risk for
high blood lead levels in the US. Low-income
people often live in old housing with lead paint, which may begin to peel, exposing
residents to high levels of lead-containing dust.
Risk factors for
elevated lead exposure include alcohol consumption and smoking (possibly
because of contamination of tobacco leaves with lead-containing pesticides).[168] Adults with
certain risk factors might be more susceptible to toxicity; these include
calcium and iron deficiencies, old age, disease of organs targeted by lead (e.g.
the brain, the kidneys), and possibly genetic susceptibility.] Differences
in vulnerability to lead-induced neurological damage between males and females
have also been found, but some studies have found males to be at greater risk,
while others have found females to be.
In adults, blood
lead levels steadily increase with increasing age. In adults of all ages, men
have higher blood lead levels than women do. Children
are more sensitive to elevated blood lead levels than adults are. hildren may also have a higher
intake of lead than adults; they breathe faster and may be more likely to have
contact with and ingest soil. Children of ages one to three
tend to have the highest blood lead levels, possibly because at that age they
begin to walk and explore their environment, and they use their mouths in their
exploration. Blood levels usually peak at
about 18–24 months old. In many countries including the
US, household paint and dust are the major route of exposure in children.
Notable Cases
Cases of mass
lead poisoning can occur. 15,000 people are being relocated from Jiyuan in
central Henan province to other
locations after 1000 children living around China's largest smelter plant
(owned and operated by Yuguang Gold and Lead) were found to have excess lead in
their blood. The total cost of this project is estimated to around
1 billion yuan ($150 million). 70% of the cost will be paid by local
government and the smelter company, while the rest will be paid by the
residents themselves. The government has suspended production at 32 of 35 lead
plants. The affected area includes people from 10 different villages.
The Zamfara State lead poisoning epidemic occurred in
Nigeria in 2010. As of 5 October 2010 at least 400 children have died from the
effects of lead poisoning.
Sex-specific susceptibility Neuroanatomical pathology due
to lead exposure is more pronounced in males, suggesting that lead-related
toxicity has a disparate impact across sexes .
Prognosis
Reversibility
Outcome is
related to the extent and duration of lead exposure. Effects of
lead on the physiology of the kidneys and blood are generally reversible; its
effects on the central nervous system are not. While peripheral effects in
adults often go away when lead exposure ceases, evidence suggests that most of
lead's effects on a child's central nervous system are irreversible. Children with lead poisoning may
thus have adverse health, cognitive, and behavioral effects that follow them
into adulthood.
Encephalopathy
Lead
encephalopathy is a medical emergency and causes permanent brain damage in
70–80% of children affected by it, even those that receive the best treatment.] The
mortality rate for people who develop cerebral involvement is about 25%, and of
those who survive who had lead encephalopathy symptoms by the time chelation
therapy was begun, about 40% have permanent neurological problems such as cerebral
palsy.
Long-term
Exposure to lead
may also decrease lifespan and have health effects in the long term. Death rates from a
variety of causes have been found to be higher in people with elevated blood
lead levels; these include cancer, stroke, and heart disease, and general death
rates from all causes. Lead is considered a possible human carcinogen based on
evidence from animal studies. Evidence also suggests
that age-related mental decline and psychiatric symptoms are correlated with
lead exposure. Cumulative exposure over a prolonged period may have a more
important effect on some aspects of health than recent exposure. Some
health effects, such as high blood pressure, are only
significant risks when lead exposure is prolonged (over about one year). Furthermore,
the neurological effects of lead exposure have been shown to be exacerbated and
long lasting in low income children in comparison to those of higher economic
standing. ] This does
not imply that being wealthy can prevent lead from causing long-term mental
health issues.
Violence
Lead poisoning in
children has been linked to changes in brain function that can result in
low IQ, and increased
impulsivity and aggression. These traits of childhood lead exposure are
associated with crimes of passion, such as aggravated assault in young adults. An
increase in lead exposure in children was linked to an increase in aggravated
assault rates 22 years later. For
instance, the peak in leaded
gasoline use in the late 1970s
corresponds to a peak in aggravated assault rates in the late 1990s in urban
areas across the United States.
Dioscorides noted
lead's effect on the mind in the first century AD.
Roman lead water pipes with taps
Lead poisoning
was among the first known and most widely studied work regarding environmental hazards. One of the
first metals to be smelted and
used, lead is thought to have been discovered and first mined in Anatolia around 6500
BC. Its
density, workability, and corrosion resistance were among the metal's
attractions.
In the 2nd century BC the Greek botanist Nicander described the colic and paralysis seen in lead-poisoned people. Dioscorides, a Greek physician who lived in the 1st century AD, wrote that lead makes the mind "give way".
Lead was used
extensively in Roman aqueducts from
about 500 BC to 300 AD. Julius Caesar's
engineer, Vitruvius, reported,
"water is much more wholesome from earthenware pipes than
from lead pipes. For it seems to be made injurious by lead, because white lead is produced
by it, and this is said to be harmful to the human body." Gout, prevalent in
affluent Rome, is thought to be the result of lead, or leaded eating and
drinking vessels. Sugar of lead (lead acetate) was used to
sweeten wine, and the gout that resulted from this was known as
"saturnine" gout. It is even hypothesized that
lead poisoning may have contributed to the decline of the Roman Empire, a
hypothesis thoroughly disputed:
The great disadvantage of lead has always been that it is
poisonous. This was fully recognized by the ancients, and Vitruvius
specifically warns against its use. Because it was nevertheless used in
profusion for carrying drinking water, the conclusion has often been drawn that
the Romans must therefore have suffered from lead poisoning; sometimes conclusions
are carried even further and it is inferred that this caused infertility and
other unwelcome conditions, and that lead plumbing was largely responsible for
the decline and fall of Rome. Two things make this otherwise attractive
hypothesis impossible. First, the calcium carbonate deposit
that formed so thickly inside the aqueduct channels
also formed inside the pipes, effectively insulating the water from the lead,
so that the two never touched. Second, because the Romans had so few taps and the
water was constantly running, it was never inside the pipes for more than a few
minutes, and certainly not long enough to become contaminated.
However, recent
research supports the idea that the lead found in the water came from the
supply pipes, rather than another source of contamination. It was not unknown
for locals to punch holes in the pipes to draw water off, increasing the number
of people exposed to the lead.
Thirty years ago, Jerome Nriagu argued in a milestone
paper that Roman civilization collapsed as a result of lead poisoning. Clair Patterson, the scientist
who convinced governments to ban lead from gasoline, enthusiastically endorsed
this idea, which nevertheless triggered a volley of publications aimed at
refuting it. Although today lead is no longer seen as the prime culprit of
Rome's demise, its status in the system of water distribution by lead pipes
(fistulæ) still stands as a major public health issue. By measuring Pb isotope
compositions of sediments from the Tiber River and the Trajanic Harbor, the
present work shows that "tap water" from ancient Rome had 100 times
more lead than local spring waters.
Romans also
consumed lead through the consumption of defrutum,
carenum, and sapa, musts made by
boiling down fruit in lead cookware. Defrutum and its relatives were used
in ancient Roman cuisine and
cosmetics, including as a food preservative. The use of
leaden cookware, though popular, was not the general standard and copper
cookware was used far more generally. There is also no indication how often
sapa was added or in what quantity.
The consumption of sapa as having a role in the fall of the Roman Empire was used in a theory proposed by geochemist Jerome Nriagu to state that "lead poisoning contributed to the decline of the Roman Empire". In 1984, John Scarborough, a pharmacologist and classicist, criticized the conclusions drawn by Nriagu's book as "so full of false evidence, miscitations, typographical errors, and a blatant flippancy regarding primary sources that the reader cannot trust the basic arguments."
After antiquity, mention of lead
poisoning was absent from medical literature until the
end of the Middle Ages.[260] In 1656 the
German physician Samuel Stockhausen recognized
dust and fumes containing lead compounds as the cause of disease, called since
ancient Roman times morbi metallici, that were known to afflict
miners, smelter workers, potters, and others
whose work exposed them to the metal.
The painter Caravaggio might have
died of lead poisoning. Bones with high lead levels were recently found in a
grave thought likely to be his. Paints used at the time contained high
amounts of lead salts. Caravaggio is known to have exhibited violent behavior,
a symptom commonly associated with lead poisoning.
In 17th-century
Germany, the physician Eberhard
Gockel discovered lead-contaminated
wine to be the cause of an epidemic of colic. He had noticed that monks
who did not drink wine were healthy, while wine drinkers developed colic, and
traced the cause to sugar of lead, made by simmering litharge with
vinegar. As a result, Eberhard Ludwig, Duke of Württemberg issued
an edict in 1696
banning the adulteration of wines with litharge.
In the 18th
century lead poisoning was fairly frequent on account of the widespread
drinking of rum, which was made
in stills with a lead
component (the "worm"). It was a significant cause of mortality
amongst slaves and sailors in the colonial West Indies. Lead poisoning from rum
was also noted in Boston. Benjamin Franklin suspected
lead to be a risk in 1786. Also in the 18th century, "Devonshire colic" was the name
given to the symptoms experienced by people of Devon who drank
cider made in presses that were
lined with lead. Lead was added to cheap wine illegally in the 18th and early
19th centuries as a sweetener. The
composer Beethoven, a heavy wine
drinker, had elevated lead levels (as later detected in his hair) possibly due to
this; the cause of his death is controversial, but lead poisoning is a
contender as a factor.
With the Industrial Revolution in the 19th
century, lead poisoning became common in the work setting. The introduction of
lead paint for residential use in the 19th century increased childhood exposure
to lead; for millennia before this, most lead exposure had been occupational. The first legislation in the UK to limit
pottery workers' exposure to lead was included in the Factories Act Extension Act in
1864, with further introduced in 1899.William
James Furnival (1853–1928), research
ceramist of City & Guilds London Institute, appeared before Parliament in
1901 and presented a decade's evidence to convince the nation's leaders to
remove lead completely from the British ceramic industry. His 852-page
treatise, Leadless Decorative Tiles, Faience, and Mosaic of
1904 published that campaign and provided recipes to promote lead-free
ceramics. At the request of the Illinois state government in the US, Alice
Hamilton (1869–1970) documented lead
toxicity in Illinois industry and in 1911 presented results to the 23rd Annual
Meeting of the American Economic Association. Hamilton was a founder of
the field of occupational safety and health and
published the first edtion of her manual, Industrial Toxicology in
1934, yet in print in revised forms.[274] An
important step in the understanding of childhood lead poisoning occurred
when toxicity in children
from lead paint was recognized in Australia in 1897. France, Belgium, and
Austria banned white lead interior paints in 1909; the League of Nations followed
suit in 1922 However, in the United States, laws banning lead house paint
were not passed until 1971,and it was phased out and not fully banned until
1978.
The 20th century saw an increase in worldwide lead exposure levels due to the increased widespread use of the metal. Begnning in the 1920s, lead was added to gasoline to improve its combustion; lead from this exhaust persists today in soil and dust in buildings Midcentury ceramicist Carol Janeway provides a case history of lead poisoning in an artist using lead glazes in decorating tiles in the 1940s; her monograph suggests that other artists' potential for lead poisoning be investigated, for example Vally Wieselthier and Dora Carrington. Blood lead levels worldwide have been declining sharply since the 1980s, when leaded gasoline began to be phased out of those countries that have banned lead in solder for food and drink cans and have banned leaded gasoline additives, blood lead levels have fallen sharply since the mid-1980s.
The levels found
today in most people are orders of magnitude greater than those of pre-industrial society. Due to
reductions of lead in products and the workplace, acute lead poisoning is rare
in most countries today, but low-level lead exposure is still common. It
was not until the second half of the 20th century that subclinical lead
exposure became understood to be a problem. During the end of the 20th century, the blood
lead levels deemed acceptable steadily decline Blood lead
levels once considered safe are now considered hazardous, with no known safe
threshold.
In the late 1950s through the 1970s Herbert Needleman and Clair Cameron Patterson did research trying to prove lead's toxicity to humans in the 1980s Needleman was falsely accused of scientific misconduct by the lead industry associate.
In 2002 Tommy Thompson, secretary of Health and Human Services appointed at least two persons with conflicts of interest to the CDC's Lead Advisory Coittee.
In 2014 a case by
the state of California against a number of companies decided against Sherwin-Williams, NL Industries and ConAgra and ordered
them to pay $1.15 billion. The
disposition of The People v. ConAgra Grocery Products Company et al. in
the California 6th Appellate District Court on 14 November 2017 is that:
... the judgment is reversed, and the matter is remanded
to the trial court with directions to recalculate the amount of the
abatement fund to limit it to the amount necessary to cover the cost of
remediating pre-1951 homes, and hold an evidentiary hearing regarding the
appointment of a suitable receiver. The Plaintiff shall recover its costs on
appeal.
On 6 December 2017, the petitions for rehearing from NL Industries, Inc., ConAgra Grocery Products Company and The Sherwin-Williams Company were denied.
Studies have
found a weak link between lead from leaded gasoline and crime rates.
As of
2022 in the United States lead paint in rental housing remains a hazard to
children. Both landlords and insurance companies have adopted strategies which
limit the chance of recovery for damages due to lead poisoning: insurance
companies by excluding coverage for lead poisoning from policies and landlords
by crafting barriers to collection of any money damages compensating plaintiffs
for damage.
Wildlife
Turkey vultures, Cathartes
aura (shown), and California condors can be
poisoned when they eat carcasses of animals shot with lead pellets.
Lead, one of the
leading causes of toxicity in waterfowl, has been known to cause die-offs of
wild bird populations. When hunters use lead shot, waterfowl such as
ducks can ingest the spent pellets later and be poisoned; predators that eat
these birds are also at risk. Lead shot-related waterfowl
poisonings were first documented in the US in the 1880s. By 1919, the spent lead
pellets from waterfowl hunting was positively identified as the source of
waterfowl deaths. Lead shot has been banned for hunting
waterfowl in several countries, including the US in 1991 and Canada in 1997.
Other threats to wildlife include lead paint,
sediment from lead mines and smelters, and lead weights from fishing lines. Lead in
some fishing gear has been banned in several countries.
The critically endangered California condor has also
been affected by lead poisoning. As scavengers, condors eat
carcasses of game that have been shot but not retrieved, and with them the
fragments from lead bullets; this increases their lead levels. Among
condors around the Grand Canyon, lead poisoning
due to eating lead shot is the most frequently diagnosed cause of
death. In an effort to protect this species, in areas designated as the
California condor's range the use of projectiles containing lead has been
banned to hunt deer, feral pigs, elk, pronghorn antelope, coyotes, ground
squirrels, and other non-game wildlife. Also,
conservation programs exist which routinely capture condors, check their blood
lead levels, and treat cases of poisoning.
Jan Ricks
Jennings, MHA, LFACHE
Senior Consultant
Senior Management
Resources LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
October 21, 2023


















No comments:
Post a Comment