Asperger
syndrome (AS)
Asperger syndrome (AS), also known as Asperger's, was the name of a neurodevelopmental disorder no longer recognized as a diagnosis, having been merged into autism spectrum dis
order (ASD). It was characterized by significant difficulties in social interaction and nonverbal communication, along with restricted and repetitive patterns of behavior and interests. It was said to differ from other diagnoses that were merged into ASD by relatively unimpaired language and intelligence. The syndrome was named after the Austrian pediatrician Hans Asperger, who, in 1944, described children in his care who struggled to form friendships, did not understand others' gestures or feelings, engaged in one-sided conversations about their favorite interests, and were clumsy.
The exact cause of
Asperger's is poorly understood. While
it has high heritability, the underlying genetics have not been determined conclusively. Environmental factors are also believed to
play a role. Brain imaging has not identified a common underlying condition.
In 1994, the diagnosis of
Asperger's was included in the fourth edition (DSM-IV) of the American
Diagnostic and Statistical Manual of Mental Disorders; with the publication of
DSM-5 in 2013 the diagnosis was removed, and the symptoms are now included
within autism spectrum disorder along with classic autism and pervasive
developmental disorder not otherwise specified (PDD-NOS). It was similarly merged into autism spectrum
disorder in the International Classification of Diseases (ICD-11) as of 2021.
There is no single
treatment, and the UK's National Health Service (NHS) guidelines suggest that
'treatment' of any form of autism should not be a goal, since autism is not 'a
disease that can be removed or cured'. According
to the Royal College of Psychiatrists, while co-occurring conditions might require
treatment, 'management of autism itself is chiefly about the provision of the
education, training and social support/care required to improve the person's
ability to function in the everyday world'. The effectiveness of particular
interventions for autism is supported by only limited data. Interventions may
include social skills training, cognitive behavioral therapy, physical therapy,
speech therapy, parent training, and medications for associated problems, such
as mood or anxiety. Autistic
characteristics tend to become less obvious in adulthood, but social and
communication difficulties usually persist.
Some autistic people, as
well as a number of researchers, have advocated a shift in attitudes toward the
view that autism spectrum disorder is a difference, rather than a disease that
must be treated or cured. Critics have
bemoaned the entrenchment of some of these groups' opinions.
In 2015, Asperger's was
estimated to affect 37.2 million people globally, about 0.5% of the population.
The exact percentage of people affected
is not firmly established. Autism spectrum
disorder is diagnosed in males more often than females,[33] and females are
typically diagnosed at a later age. The modern conception of Asperger syndrome
came into existence in 1981, and went through a period of popularization. It became a standardized diagnosis in the
1990s, and was retired as a diagnosis in 2013. Many questions and controversies about the
condition remain.
The extent of the overlap
between Asperger syndrome and high-functioning autism (HFA – autism
unaccompanied by intellectual disability) is unclear. The ASD classification is to some extent an
artifact of how autism was discovered,[43] and may not reflect the true nature
of the spectrum; methodological problems have beset Asperger syndrome as a
valid diagnosis from the outset.[45][46] In the fifth edition of the Diagnostic
and Statistical Manual of Mental Disorders (DSM-5), published in May 2013,
Asperger syndrome, as a separate diagnosis, was eliminated and folded into
autism spectrum disorder. Like the diagnosis of Asperger syndrome, the change
was controversial and thus Asperger syndrome was subsequently not removed from
the WHO's ICD-10; however, it was removed from the ICD-11.
The World Health
Organization (WHO) previously defined Asperger syndrome (AS) as one of the autism
spectrum disorders (ASD) or pervasive developmental disorders (PDD), which are
a spectrum of psychological conditions that are characterized by abnormalities
of social interaction and communication that pervade the individual's
functioning, and by restricted and repetitive interests and behavior. Like
other neurodevelopment disorders, ASD begins in infancy or childhood, has a
steady course without remission or relapse, and has impairments that result
from maturation-related changes in various systems of the brain. ASD, in turn,
is a subset of the broader autism phenotype, which describes individuals who
may not have ASD but do have autistic-like traits, such as social deficits.
Characteristics
A young boy is seen stacking
several colorful cans on top of each other.
People with Asperger
syndrome often display restricted or specialized interests, such as this boy's
interest in stacking cans.
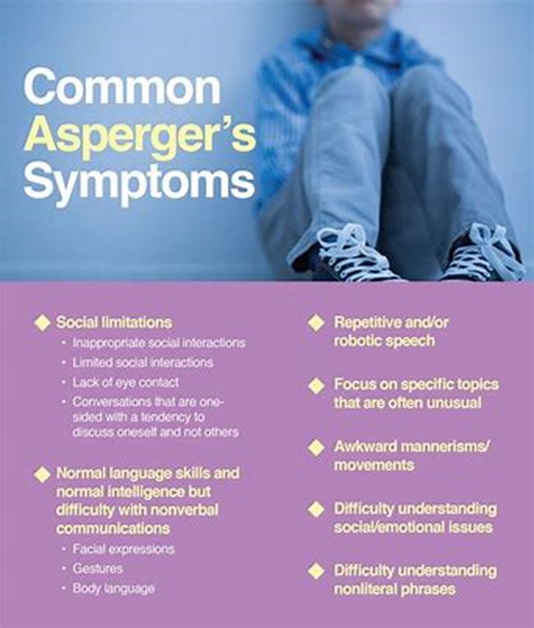
As a pervasive developmental
disorder, Asperger syndrome is distinguished by a pattern of symptoms rather
than a single symptom. It is characterized by qualitative impairment in social
interaction, by stereotyped and restricted patterns of behavior, activities,
and interests, and by no clinically significant delay in cognitive development
or general delay in language.[55] Intense preoccupation with a narrow subject,
one-sided verbosity, restricted prosody, and physical clumsiness are typical of
the condition, but are not required for diagnosis.[40] Suicidal behavior
appears to occur at rates similar to those without ASD.[56]
Social interaction
Further information:
Asperger syndrome and interpersonal relationships
A lack of demonstrated
empathy affects aspects of social relatability for persons with Asperger
syndrome. Individuals with Asperger syndrome experience
difficulties in basic elements of social interaction, which may include a
failure to develop friendships or to seek shared enjoyments or achievements
with others (e.g., showing others objects of interest); a lack of social or
emotional reciprocity (social "games" give-and-take mechanic); and
impaired nonverbal behaviors in areas such as eye contact, facial expression,
posture, and gesture.
People with Asperger
syndrome may not be as withdrawn around others, compared with those with other
forms of autism; they approach others, even if awkwardly. For example, a person
with Asperger syndrome may engage in a one-sided, long-winded speech about a
favorite topic, while misunderstanding or not recognizing the listener's
feelings or reactions, such as a wish to change the topic of talk or end the
interaction.[40] This social awkwardness has been called "active but
odd". Such failures to react appropriately to social interaction may
appear as disregard for other people's feelings and may come across as rude or
insensitive. However, not all
individuals with Asperger syndrome will approach others. Some may even display
selective mutism, not speaking at all to most people and excessively to
specific others. Some may choose only to talk to people they like.
The cognitive ability of
children with AS often allows them to articulate social norms in a laboratory
context, where they may be able to show a theoretical understanding of other
people's emotions; however, they typically have difficulty acting on this
knowledge in fluid, real-life situations. People with AS may analyze and distill their
observations of social interaction into rigid behavioral guidelines and apply
these rules in awkward ways, such as forced eye contact, resulting in a
demeanor that appears rigid or socially naïve. Childhood desire for
companionship can become numbed through a history of failed social encounters.
Violent or criminal behavior
The hypothesis that
individuals with AS are predisposed to violent or criminal behavior has been
investigated but is not supported by data. More evidence suggests that children diagnosed
with Asperger syndrome are more likely to be victims, rather than offenders.
A 2008 review found that an
overwhelming number of reported violent criminals with Asperger syndrome also
had other coexisting psychotic psychiatric disorders such as schizoaffective
disorder. This coexistence of psychotic
disorders is referred to as comorbid disorders. Comorbid disorders can be
completely independent of one another or can have overlap in symptoms and how
they express themselves.
Empathy
People with an Asperger
profile might not be recognized for their empathetic qualities, due to
variation in the ways empathy is felt and expressed. Some people feel deep
empathy, but do not outwardly communicate these sentiments through facial
expressions or language. Some people come to empathy through intellectual
processes, using logic and reasoning to arrive at the feelings. It is also
important to keep in mind that many people with Asperger profiles have been
bullied or excluded by peers in the past and might therefore be guarded around
people, which could appear as lack of empathy. People with Asperger profiles
can be and are extremely caring individuals; in fact, it is particularly common
for those with the profile to feel and exhibit deep concern for human welfare,
animal rights, environmental protection, and other global and humanitarian
causes.
Evidence suggests that in
the "double empathy problem model, autistic people have a unique
interaction style which is significantly more readable by other autistic
people, compared to non-autistic people."
Restricted and repetitive
interests and behavior
People with Asperger
syndrome can display behavior, interests, and activities that are restricted
and repetitive and are sometimes abnormally intense or focused. They may stick
to inflexible routines, move in stereotyped and repetitive ways, preoccupy
themselves with parts of objects, or engage in compulsive behaviors like lining
objects up to form patterns.
The pursuit of specific and
narrow areas of interest is one of the most striking among possible features of
AS. Individuals with AS may collect
volumes of detailed information on a relatively narrow topic such as weather
data or star names without necessarily having a genuine understanding of the
broader topic. For example, a child
might memorize camera model numbers while caring little about photography. This
behavior is usually apparent by age 5 or 6.
Although these special interests may change from time to time, they
typically become more unusual and narrowly focused and often dominate social
interaction so much that the entire family may become immersed. Because narrow
topics often capture the interest of children, this symptom may go
unrecognized.
Stereotyped and repetitive
motor behaviors are a core part of the diagnosis of AS and other ASDs. They include hand movements such as flapping
or twisting, and complex whole-body movements. These are typically repeated in longer bursts
and look more voluntary or ritualistic than tics, which are usually faster, less
rhythmical, and less often symmetrical. However, in addition to this, various studies
have reported a consistent comorbidity between AS and Tourette syndrome in the
range of 8–20%, with one figure as high as 80% for tics of some kind or
another, for which several explanations have been put forward, including common
genetic factors and dopamine, glutamate, or serotonin abnormalities.
According to the Adult
Asperger Assessment (AAA) diagnostic test, a lack of interest in fiction and a
positive preference towards non-fiction is common among adults with AS.
Speech and language
Although individuals with
Asperger syndrome acquire language skills without significant general delay and
their speech typically lacks significant abnormalities, language acquisition
and use is often atypical. Abnormalities
include verbosity; abrupt transitions; literal interpretations and
miscomprehension of nuance; use of metaphor meaningful only to the speaker;
auditory perception deficits; unusually pedantic, formal, or idiosyncratic
speech; and oddities in loudness, pitch, intonation, prosody, and rhythm. Echolalia has also been observed in
individuals with AS.
Three aspects of
communication patterns are of clinical interest: poor prosody, tangential and
circumstantial speech, and marked verbosity. Although inflection and intonation
may be less rigid or monotonic than in classic autism, people with AS often
have a limited range of intonation: speech may be unusually fast, jerky, or
loud. Speech may convey a sense of incoherence; the conversational style often
includes monologues about topics that bore the listener, fails to provide
context for comments, or fails to suppress internal thoughts. Individuals with
AS may fail to detect whether the listener is interested or engaged in the
conversation. The speaker's conclusion or point may never be made and attempts
by the listener to elaborate on the speech's content or logic, or to shift to
related topics, are often unsuccessful.
Children with AS may have a sophisticated
vocabulary at a young age and such children have often been colloquially called
"little professors"[75] but have difficulty understanding figurative
language and tend to use language literally.[18] Children with AS appear to
have particular weaknesses in areas of nonliteral language that include humor,
irony, teasing, and sarcasm. Although individuals with AS usually understand
the cognitive basis of humor, they seem to lack understanding of the intent of
humor to share the enjoyment with others.[41] Despite strong evidence of
impaired humor appreciation, anecdotal reports of humor in individuals with AS
seem to challenge some psychological theories of AS and autism.[76]
Motor and sensory perception
Individuals with Asperger
syndrome may have signs or symptoms that are independent of the diagnosis but
can affect the individual or the family.
These include differences in perception and problems with motor skills,
sleep, and emotions.
Individuals with AS often
have excellent auditory and visual perception.
Children with ASD often
demonstrate enhanced perception of small changes in patterns such as
arrangements of objects or well-known images; typically this is domain-specific
and involves processing of fine-grained features. Conversely, compared with individuals with
high-functioning autism, individuals with AS have deficits in some tasks
involving visual-spatial perception, auditory perception, or visual memory. Many accounts of individuals with AS and ASD
report other unusual sensory and perceptual skills and experiences. They may be
unusually sensitive or insensitive to sound, light, and other stimuli;[80]
these sensory responses are found in other developmental disorders and are not
specific to AS or to ASD. There is little support for increased fight-or-flight
response or failure of habituation in autism; there is more evidence of
decreased responsiveness to sensory stimuli, although several studies show no
differences.
Hans Asperger's initial
accounts and other diagnostic scheme. include
descriptions of physical clumsiness. Children with AS may be delayed in
acquiring skills requiring dexterity, such as riding a bicycle or opening a
jar, and may seem to move awkwardly or feel "uncomfortable in their own
skin". They may be poorly coordinated or have an odd or bouncy gait or
posture, poor handwriting, or problems with motor coordination. They may show
problems with proprioception (sensation of body position) on measures of
developmental coordination disorder (motor planning disorder), balance, tandem
gait, and finger-thumb apposition. There is no evidence that these motor skills
problems differentiate AS from other high-functioning ASDs.
Children with AS are more
likely to have sleep problems, including difficulty in falling asleep, frequent
nocturnal awakenings, and early morning awakenings. AS is also associated with
high levels of alexithymia, which is difficulty in identifying and describing
one's emotions. Although AS, lower sleep quality, and alexithymia are
associated with each other, their causal relationship is unclear.
Causes
Further information: Causes
of autism
Hans Asperger described
common traits among his patients' family members, especially fathers, and
research supports this observation and suggests a genetic contribution to
Asperger syndrome. Although no specific genetic factor has yet been identified,
multiple factors are believed to play a role in the expression of autism, given
the variability in symptoms seen in children. Evidence for a genetic link is that AS tends
to run in families where more family members have limited behavioral symptoms
similar to AS (for example, some problems with social interaction, or with
language and reading skills). Most
behavioral genetic research suggests that all autism spectrum disorders have
shared genetic mechanisms, but AS may have a stronger genetic component than
autism. There may be shared genes in which particular alleles make an
individual vulnerable, and varying combinations result in differing severity
and symptoms in each person with AS.
A few ASD cases have been
linked to exposure to teratogens (agents that cause birth defects) during the
first eight weeks from conception. Although this does not exclude the
possibility that ASD can be initiated or affected later, it is strong evidence
that ASD arises very early in development. Many environmental factors have been
hypothesized to act after birth, but none has been confirmed by scientific
investigation.
Mechanism
Further information: Autism
§ Mechanism
Monochrome fMRI image of a
horizontal cross-section of a human brain. A few regions, mostly to the rear,
are highlighted in orange and yellow.
Functional magnetic
resonance imaging provides some evidence for mirror neuron theory.
Asperger syndrome appears to
result from developmental factors that affect many or all functional brain
systems, as opposed to localized effects.
Although the specific
underpinnings of AS or factors that distinguish it from other ASDs are unknown,
and no clear pathology common to individuals with AS has emerged, it is still
possible that AS's mechanism is separate from other ASDs.
Neuroanatomical studies and
the associations with teratogens strongly suggest that the mechanism includes
alteration of brain development soon after conception. Abnormal fetal
development may affect the final structure and connectivity of the brain,
resulting in altered neural circuits controlling thought and behavior. Several
theories of mechanism are available; none are likely to provide a complete
explanation.
General-processing theories
One general-processing
theory is weak central coherence theory, which hypothesizes that a limited
ability to see the big picture underlies the central disturbance in ASD. A related theory—enhanced perceptual
functioning—focuses more on the superiority of locally oriented and perceptual
operations in autistic individuals.
Mirror neuron system (MNS)
theory
Ambox current red.svg
This section's factual
accuracy may be compromised due to out-of-date information. The reason given
is: There have been almost 4 decades since some of the material cited here was
published, and current consensus in ASD is less straightforward than depicted
here. Please help update this article to reflect recent events or newly
available information. (January 2022)
The mirror neuron system
(MNS) theory hypothesizes that alterations to the development of the MNS
interfere with imitation and lead to Asperger's core feature of social
impairment. One study found that
activation is delayed in the core circuit for imitation in individuals with AS.
This theory maps well to social
cognition theories like the theory of mind, which hypothesizes that autistic
behavior arises from impairments in ascribing mental states to oneself and
others; or hyper-systemizing, which hypothesizes that autistic individuals can
systematize internal operation to handle internal events but are less effective
at empathizing when handling events generated by other agents.
Diagnosis
Main article: Diagnosis of
Asperger syndrome
Standard diagnostic criteria
require impairment in social interaction and repetitive and stereotyped
patterns of behavior, activities, and interests, without significant delay in
language or cognitive development. Unlike the international standard,[53] the
DSM-IV-TR criteria also required significant impairment in day-to-day
functioning; DSM-5 eliminated AS as a separate diagnosis in 2013, and folded it
into the umbrella of autism spectrum disorders. Other sets of diagnostic criteria have been
proposed by Szatmari et al. and by Gillberg and Gillberg.
Diagnosis is most commonly
made between the ages of four and eleven. A comprehensive assessment involves a
multidisciplinary team that observes across multiple settings, and includes
neurological and genetic assessment as well as tests for cognition, psychomotor
function, verbal and nonverbal strengths and weaknesses, style of learning, and
skills for independent living. The "gold standard" in diagnosing ASDs
combines clinical judgment with the Autism Diagnostic Interview-Revised
(ADI-R), a semi structured parent interview; and the Autism Diagnostic
Observation Schedule (ADOS), a conversation and play-based interview with the
child. Delayed or mistaken diagnosis can
be traumatic for individuals and families; for example, misdiagnosis can lead
to medications that worsen behavior.
Underdiagnosis and
overdiagnosis may be problems. The cost and difficulty of screening and
assessment can delay diagnosis. Conversely, the increasing popularity of drug
treatment options and the expansion of benefits has motivated providers to
overdiagnose ASD. There are indications
AS has been diagnosed more frequently in recent years, partly as a residual
diagnosis for children of normal intelligence who are not autistic but have
social difficulties.
There are questions about the
external validity of the AS diagnosis. That is, it is unclear whether there is
a practical benefit in distinguishing AS from HFA and from PDD-NOS; different screening tools render different
diagnoses depending in the same person.
Differential diagnosis
Many children with AS are
initially misdiagnosed with attention deficit hyperactivity disorder (ADHD). Diagnosing adults is more challenging, as
standard diagnostic criteria are designed for children and the expression of AS
changes with age. Adult diagnosis
requires painstaking clinical examination and thorough medical history gained
from both the individual and other people who know the person, focusing on
childhood behavior.
Conditions that must be
considered in a differential diagnosis along with ADHD include other ASDs, the
schizophrenia spectrum, personality disorders, obsessive–compulsive disorder,
major depressive disorder, semantic pragmatic disorder, nonverbal learning
disorder, social anxiety disorder, Tourette syndrome,[68] stereotypic movement
disorder, bipolar disorder,[86] social-cognitive deficits due to brain damage
from alcohol use disorder, and obsessive–compulsive personality disorder
(OCPD).
Screening
Parents of children with
Asperger syndrome can typically trace differences in their children's
development to as early as 30 months of age.
Developmental screening during a routine check-up by a general
practitioner or pediatrician may identify signs that warrant further
investigation. The United States
Preventive Services Task Force in 2016 found it was unclear if screening was
beneficial or harmful among children in whom there are no concerns.
Different screening
instruments are used to diagnose AS, including the Asperger Syndrome Diagnostic
Scale (ASDS); Autism Spectrum Screening Questionnaire (ASSQ); Childhood Autism
Spectrum Test (CAST), previously called the Childhood Asperger Syndrome Test;
Gilliam Asperger's disorder scale (GADS); Krug Asperger's Disorder Index
(KADI); and the autism-spectrum quotient (AQ), with versions for children,
adolescents, and adults. None have been shown to reliably differentiate between
AS and other ASDs.
Management
Further information: Autism
therapies
Asperger syndrome treatment
attempts to manage distressing symptoms and to teach age-appropriate social,
communication, and vocational skills that are not naturally acquired during development,
with intervention tailored to the needs of the individual based on
multidisciplinary assessment. Although
progress has been made, data supporting the efficacy of particular
interventions are limited.
Therapies
Managing AS ideally involves
multiple therapies that address core symptoms of the disorder. While most
professionals agree that the earlier the intervention, the better, there is no
treatment combination that is recommended above others. AS treatment resembles that of other
high-functioning ASDs, except that it takes into account the linguistic
capabilities, verbal strengths, and nonverbal vulnerabilities of individuals
with AS. A typical program generally includes:
Applied behavior analysis
(ABA) procedures, including positive behavior support (PBS)—or training and
support of parents and school faculty in behavior management strategies to use
in the home and school, and social skills training for more effective
interpersonal interactions;
Cognitive behavioral therapy
to improve stress management relating to anxiety or explosive emotions and to
help reduce obsessive interests and repetitive routines;
Medication for coexisting
conditions such as major depressive disorder and anxiety disorders;
Occupational or physical
therapy to assist with poor sensory processing and motor coordination; and,
Social communication
intervention, which is specialized speech therapy to help with the pragmatics
and give-and-take of normal conversation.
Of the many studies on
behavior-based early intervention programs, most are case reports of up to five
participants and typically examine a few problem behaviors such as self-injury,
aggression, noncompliance, stereotypies, or spontaneous language; unintended
side effects are largely ignored. Despite the popularity of social skills
training, its effectiveness is not firmly established. A randomized controlled
study of a model for training parents in problem behaviors in their children
with AS showed that parents attending a one-day workshop or six individual lessons
reported fewer behavioral problems, while parents receiving the individual
lessons reported less intense behavioral problems in their AS children. Vocational training is important to teach job
interview etiquette and workplace behavior to older children and adults with
AS, and organization software and personal data assistants can improve the work
and life management of people with AS.
Medications
No medications directly
treat the core symptoms of AS. Although research into the efficacy of
pharmaceutical intervention for AS is limit, it is essential to diagnose and
treat comorbid conditions. Deficits in self-identifying emotions or in
observing effects of one's behavior on others can make it difficult for
individuals with AS to see why medication may be appropriate. Medication can be
effective in combination with behavioral interventions and environmental
accommodations in treating comorbid symptoms such as anxiety disorders, major
depressive disorder, inattention, and aggression. The atypical antipsychotic
medications risperidone, olanzapine and aripiprazole have been shown to reduce
the associated symptoms of AS; risperidone can reduce repetitive and
self-injurious behaviors, aggressive outbursts, and impulsivity, and improve
stereotypical patterns of behavior and social relatedness. The selective
serotonin reuptake inhibitors (SSRIs) fluoxetine, fluvoxamine, and sertraline
have been effective in treating restricted and repetitive interests and behaviors,
while stimulant medication, such as methylphenidate, can reduce inattention.
Care must be taken with
medications, as side effects may be more common and harder to evaluate in
individuals with AS, and tests of drugs' effectiveness against comorbid
conditions routinely exclude individuals from the autism spectrum.[120]
Abnormalities in metabolism, cardiac conduction times, and an increased risk of
type 2 diabetes have been raised as concerns with antipsychotic medications, along
with serious long-term neurological side effects..SSRIs can lead to
manifestations of behavioral activation such as increased impulsivity,
aggression, and sleep disturbance. Weight gain and fatigue are commonly reported
side effects of risperidone, which may also lead to increased risk for
extrapyramidal symptoms such as restlessness and dystonia and increased serum
prolactin levels. Sedation and weight gain are more common with olanzapine,
which has also been linked with diabetes Sedative side-effects in school-age children have
ramifications for classroom learning. Individuals with AS may be unable to
identify and communicate their internal moods and emotions or to tolerate side
effects that for most people would not be problematic.
Prognosis
There is some evidence that
children with AS may see a lessening of symptoms; up to 20% of children may no
longer meet the diagnostic criteria as adults, although social and
communication difficulties may persist. As of 2006, no studies addressing the
long-term outcome of individuals with Asperger syndrome are available and there
are no systematic long-term follow-up studies of children with AS. Individuals
with AS appear to have normal life expectancy, but have an increased prevalence
of comorbid psychiatric conditions, such as major depressive disorder and
anxiety disorders that may significantly affect prognosis. Although social
impairment may be lifelong, the outcome is generally more positive than with
individuals with lower-functioning autism spectrum disorders;[18] for example,
ASD symptoms are more likely to diminish with time in children with AS or HFA.
Most students with AS and HFA have average mathematical ability and test
slightly worse in mathematics than in general intelligence.[134] However,
mathematicians are at least three times more likely to have autism-spectrum
traits than the general population, and are more likely to have family members
with autism.
Although many attend regular
education classes, some children with AS may attend special education classes
such as separate classroom and resource room because of their social and
behavioral difficulties. Adolescents
with AS may exhibit ongoing difficulty with self-care or organization, and
disturbances in social and romantic relationships. Despite high cognitive
potential, most young adults with AS remain at home, yet some do marry and work
independently. The "different-ness" adolescents experience can be
traumatic.[136] Anxiety may stem from preoccupation over possible violations of
routines and rituals, from being placed in a situation without a clear schedule
or expectations, or from concern with failing in social encounters; the
resulting stress may manifest as inattention, withdrawal, reliance on
obsessions, hyperactivity, or aggressive or oppositional behavior. Depression is often the result of chronic
frustration from repeated failure to engage others socially, and mood disorders
requiring treatment may develop Clinical experience suggests the rate of
suicide may be higher among those with AS, but this has not been confirmed by
systematic empirical studies.
Education of families is
critical in developing strategies for understanding strengths and weaknesses;
helping the family to cope improves outcomes in children. Prognosis may be
improved by diagnosis at a younger age that allows for early interventions,
while interventions in adulthood are valuable but less beneficial There are
legal implications for individuals with AS as they run the risk of exploitation
by others and may be unable to comprehend the societal implications of their
actions.
Epidemiology
Main article: Epidemiology
of autism
Frequency estimates vary
enormously. In 2015, it was estimated that 37.2 million people globally are
affected. A 2003 review of epidemiological studies of children found autism
rates ranging from 0.03 to 4.84 per 1,000, with the ratio of autism to Asperger
syndrome ranging from 1.5:1 to 16:1; combining the geometric mean ratio of 5:1
with a conservative prevalence estimate for autism of 1.3 per 1,000 suggests
indirectly that the prevalence of AS might be around 0.26 per 1,000.[139] Part
of the variance in estimates arises from differences in diagnostic criteria.
For example, a relatively small 2007 study of 5,484 eight-year-old children in
Finland found 2.9 children per 1,000 met the ICD-10 criteria for an AS
diagnosis, 2.7 per 1,000 for Gillberg and Gillberg criteria, 2.5 for DSM-IV,
1.6 for Szatmari et al., and 4.3 per 1,000 for the union of the four criteria.
Boys seem to be more likely to have AS than girls; estimates of the sex ratio
range from 1.6:1 to 4:1, using the Gillberg and Gillberg criteria.[140] Females
with autism spectrum disorders may be underdiagnosed.
Comorbidities
Main article: Conditions
comorbid to autism spectrum disorders
Anxiety disorders and major
depressive disorder are the most common conditions seen at the same time;
comorbidity of these in persons with AS is estimated at 65%. Reports have associated AS with medical
conditions such as aminoaciduria and ligamentous laxity, but these have been
case reports or small studies and no factors have been associated with AS
across studies. One study of males with
AS found an increased rate of epilepsy and a high rate (51%) of nonverbal
learning disorder. AS is associated with tics, Tourette syndrome and bipolar
disorder. The repetitive behaviors of AS have many similarities with the
symptoms of obsessive–compulsive disorder and obsessive–compulsive personality
disorder, and 26% of a sample of young adults with AS were found to meet the
criteria for schizoid personality disorder (which is characterized by severe
social seclusion and emotional detachment), more than any other personality
disorder in the sample. However many of these studies are based on clinical
samples or lack standardized measures; nonetheless, comorbid conditions are
relatively common.
History
Main article: History of
Asperger syndrome
Named after the Austrian
pediatrician Hans Asperger (1906–1980), Asperger syndrome is a relatively new
diagnosis in the field of autism, though a syndrome like it was described as
early as 1925 by Soviet child psychiatrist Grunya Sukhareva (1891–1981),
leading some of those diagnosed with Asperger's Syndrome to instead refer to
their condition as 'Sukhareva's Syndrome', in opposition to Hans Asperger's
association with Nazism. As a child, Asperger appears to have exhibited some
features of the very condition named after him, such as remoteness and talent
in language. In 1944, Asperger described
four children in his practice who had difficulty in integrating themselves
socially and showing empathy towards peers. They also lacked nonverbal
communication skills and were physically clumsy. Asperger described this
"autistic psychopathy" as social isolation. Fifty years later,
several standardizations of AS as a medical diagnosis were tentatively proposed,
many of which diverge significantly from Asperger's original work.[149]
Unlike today's AS, autistic
psychopathy could be found in people of all levels of intelligence, including
those with intellectual disability. Asperger
defended the value of so-called "high-functioning" autistic
individuals, writing: "We are convinced, then, that autistic people have
their place in the organism of the social community. They fulfill their role
well, perhaps better than anyone else could, and we are talking of people who
as children had the greatest difficulties and caused untold worries to their caregivers."
Asperger also believed some would be capable of exceptional achievement and
original thought later in life.
Asperger's paper was
published during World War II and in German, so it was not widely read
elsewhere. Lorna Wing used the term Asperger syndrome in 1976, and popularized
it to the English-speaking medical community in her February 1981 publication
of case studies of children showing the symptoms described by Asperger, and Uta
Frith translated his paper to English in 1991. Sets of diagnostic criteria were
outlined by Gillberg and Gillberg in 1989 and by Szatmari et al. in the same
year In 1992, AS became a standard diagnosis when it was included in the tenth
edition of the World Health Organization's diagnostic manual, International
Classification of Diseases (ICD-10). It was added to the fourth edition of the
American Psychiatric Association's diagnostic reference, Diagnostic and
Statistical Manual of Mental Disorders (DSM-IV), published in 1994.
Hundreds of books, articles,
and websites now describe AS and prevalence estimates have increased
dramatically for ASD, with AS recognized as an important subgroup. Whether it should be seen as distinct from
high-functioning autism is a fundamental issue requiring further study, and
there are questions about the empirical validation of the DSM-IV and ICD-10
criteria. In 2013, DSM-5 eliminated AS as a separate diagnosis, folding it into
the autism spectrum on a severity scale.
Society and culture
See also: Societal and
cultural aspects of autism and Disability rights movement
Three children are seen
holding a banner which says "Different NOT Less! We ARE UNIFIED" in
brightly colored text.
Students and families walk
to support Autism Awareness Month.
People identifying with
Asperger syndrome may refer to themselves in casual conversation as aspies (a
term first used in print in the Boston Globe in 1998). Some
autistic people have advocated a shift in perception of autism spectrum
disorders as complex syndromes rather than diseases that must be cured.
Proponents of this view reject the notion that there is an "ideal"
brain configuration and that any deviation from the norm is pathological; they
promote tolerance for what they call neurodiversity. These views are the basis
for the autistic rights and autistic pride movements. There is a contrast
between the attitude of adults with self-identified AS, who typically do not
want to be cured and are proud of their identity; and parents of children with
AS, who typically seek assistance and a cure for their children.
Some researchers have argued
that AS can be viewed as a different cognitive style, not a disorder, and that
it should be removed from the standard Diagnostic and Statistical Manual, much
as homosexuality was removed. In a 2002 paper, Simon Baron-Cohen wrote of those
with AS: "In the social world, there is no great benefit to a precise eye
for detail, but in the worlds of maths, computing, cataloging, music,
linguistics, engineering, and science, such an eye for detail can lead to
success rather than failure." Baron-Cohen cited two reasons why it might
still be useful to consider AS to be a disability: to ensure provision for
legally required special support, and to recognize emotional difficulties from
reduced empathy.[Baron-Cohen argues that the genes for Asperger's combination
of abilities have operated throughout recent human evolution and have made
remarkable contributions to human history.
By contrast, Pier Jaarsma
and Welin wrote in 2011 that the "broad version of the neurodiversity
claim, covering low-functioning as well as high-functioning autism, is
problematic. Only a narrow conception of neurodiversity, referring exclusively
to high-functioning autists, is reasonable.
They say that "higher functioning" individuals with autism may
"not [be] benefited with such a psychiatric defect-based diagnosis ...
some of them are being harmed by it, because of the disrespect the diagnosis
displays for their natural way of being", but "think that it is still
reasonable to include other categories of autism in the psychiatric
diagnostics. The narrow conception of the neurodiversity claim should be
accepted but the broader claim should not.” Jonathan Mitchell, an autistic author and
blogger who advocates a cure for autism, has described autism as having
"prevented me from making a living or ever having a girlfriend. It is
given me bad fine motor coordination problems where I can hardly write. I have
an impaired ability to relate to people. I cannot concentrate or get things
done."[163] He describes neurodiversity as a "tempting escape
valve".
Jan Ricks Jennings, MHA,
LFACHE
Senior Consultant
Senior Management Resources,
LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
June 28, 2022