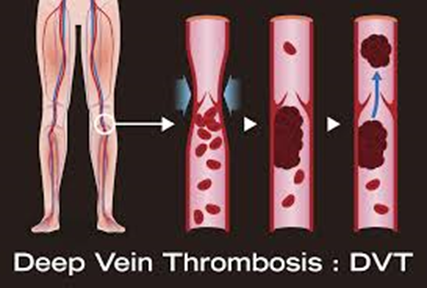
DEEP VEIN THROMBOSIS
‘Efficacy and Safety of
Early Exercise Program After Acute DVT for Prevention of Post Thrombotic
Syndrome”
The purpose of this study was
to determine the effect of exercise on patients with an acute deep vein thrombosis.
The purpose of this study is
to determine whether prescribing apixaban (Eliquis®) is more effective in
treating and preventing pulmonary embolisms and subsequent DVTs than monitoring
the calf DVT with ultrasound imaging alone.
SCD Use to Prevent DVT in
Patients with PICC Lines
Determine if the use of
sequential pneumatic compression in the arm can prevent the formation of venous
clots related to the presence of a peripherally inserted central catheter
(PICC).
A Study to Evaluate Deep
Venous Thrombus Characteristics and Venous Dynamics with Subsequent Thrombus
Resolution and Post-thrombotic Syndrome
And the purpose of this
study was to complete the following aims:
Aim 1: Evaluate initial
thrombus characteristics by ultrasound (US) shear wave elastography (SWE) in
acute, proximal, deep venous thrombus (DVT).
Aim 2: Prospectively
evaluate the role of venous hemodynamics on acute proximal DVT resolution and
post-thrombotic syndrome (PTS).
Aim 3: Examine biomarkers of
coagulation as predictors of acute proximal DVT resolution and PTS.
Aim 4: Expand the scope of
the Mayo Clinic VTE registry to include high quality outcome data on
post-thrombotic syndrome.
A Study to Identify Genes
Responsible for Venous Thromboembolism (VTE) in Families
The purpose of this study was
to identify susceptibility genes for venous thromboembolism (VTE) using
conventional and novel genetic-epidemiologic methods in high-risk VTE families.
A Study to Collect
Information about Biomarkers (Lab Test Results) that May Help to Predict Which
People with Calf Vein Clots May be at Higher or Lower Risk of Having the Clot
Grow or Progress
This is a biomarker
correlate study for a study which is randomizing patients with calf deep venous
thrombosis (calf vein clots) to treatment with blood thinners or not to see if
the blood thinner is necessary.
Intermittent Pneumatic
Compression Device Assessment in Patients with Severe Arterial and Venous
Disease of the Lower Extremity
The purpose of this study is
to determine whether a specific external compression pump called the AVT pump
can improve blood flow to the skin of the feet in patients with circulatory
problems involving the arteries or veins of the legs. The use of the AVT pump
in this study is considered investigational, which means it has either not been
approved by the Food and Drug Administration (FDA) for routine clinical use or
for the use described in this study.
Registry of Patients
Prescribed Anticoagulation
The purpose is to create a
registry of patients at Mayo Clinic who are prescribed the new novel
anticoagulation therapy with either rivaroxaban, dabigatran, apixaban, of odonatan
to allow post marketing surveillance with particular attention to cancer
patients treated with novel anticoagulants which in marketing studies the
patient numbers were small. We also want to compare efficacy and safety of
novel anticoagulants to "traditional" anticoagulants such as warfarin
and low molecular weight heparin (LMWH) and therefore to register patients
treated with this type of anticoagulation to our registry too.
Multi-Center Prospective
Validation Study of VTE Risk Prediction Tool in Trauma Patients
Almost one-half million
people suffer venous thromboembolism annually in the United States, and
one-third die from this disease. Massive bleeding from injury accounts for half
of early deaths after trauma. This study aims to prevent the deaths and
suffering associated with venous thromboembolism and bleeding by identifying
the individual person at elevated risk of these complications to take
preventive measures.
Vascular Boot Warming
Program After Acute Deep Vein Thrombosis (DVT) ± Pulmonary Embolism (PE)
The Researchers are studying
whether a vascular boot warming program plus standard of care anticoagulation
can be a safe and effective method to resolve Deep Vein Thrombosis (DVT)
±Pulmonary Embolism (PE) earlier and prevent development of post-thrombotic
syndrome (PTS). Additionally, to learn whether a more detailed imaging of the
affected lower extremities will provide a more accurate and reliable method to
guide treatment for this condition.
Apixaban in Preventing
Secondary Cancer Related Blood Clots in Cancer Patients Who Have Completed
Anticoagulation Therapy
This randomized phase III
trial studies the best dose of apixaban and how well it works in preventing
secondary cancer related blood clots in cancer patients who have completed
anticoagulation therapy. Apixaban may stop the clotting of blood by blocking
some of the enzymes needed for blood clotting.
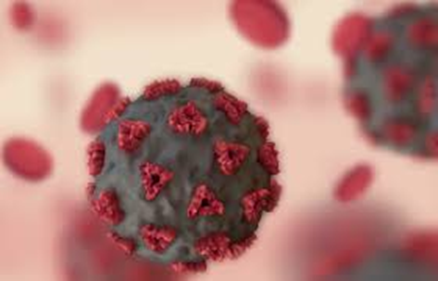
A Study to Evaluate
Rivaroxaban to Reduce Risk of Major Venous and Arterial Thrombotic Events,
Hospitalization and Death in Medically Ill Outpatients with Acute COVID-19
Infection
The purpose of this study was
to investigate the effectiveness and safety of Rivaroxaban for reducing the
risk of major venous and arterial thrombotic events, hospitalization, and death
in medically ill outpatients with acute, symptomatic COVID-19 infection.
A Study to Create and Maintain
Plasma and Serum Bank for Patients with Thrombosis
The purpose of this study is
to create and maintain a clinical database of patients with history of, or who
are at elevated risk for thromboembolic diseases, along with a plasma/serum
repository. We plan to evaluate novel biomarkers that might be associated with
thromboembolic diseases and test whether these biomarkers will help predict the
incident and recurrent recurrences of thromboembolic episodes and other
outcomes (e.g., mortality, post thrombotic syndrome).
A Study of the Safety and
Effectiveness of Apixaban in Preventing Blood Clots in Children with Leukemia
Who Have a Central Venous Catheter and Are Treated with Asparaginase
The purpose of this study is
to compare the effect of a blood thinning drug called Apixaban versus no
administration of a blood thinning drug, in preventing blood clots in children
with leukemia or lymphoma. Patients must be receiving chemotherapy, including
asparaginase, and have a central line (a catheter inserted for administration
of medications and blood sampling).
A Study to Evaluate the
Effectiveness and Safety of Rivaroxaban as Prophylaxis Treatment for Venous
Thromboembolism (VTE) in Ambulatory Cancer Patients
The purpose of this study is
to demonstrate that rivaroxaban is superior to placebo for reducing the risk of
lower extremity proximal deep vein thrombosis (DVT), asymptomatic lower
extremity proximal DVT, symptomatic upper extremity DVT, symptomatic non-fatal
pulmonary embolism (PE), incidental PE, and venous thromboembolism
(VTE)-related death in ambulatory adult patients with various cancer types
receiving systemic cancer therapy who are at high risk of developing a VTE.
.Jan Ricks Jennings, MHA,
LFACHE
Senior Consultant
Senior Management Resources,
LLC
JanJenningsBlog.Blogspot.com
724.733.0509 Office
412.913.0636 Cell
July 29, 2022