Carbon monoxide poisoning
Overview
Carbon monoxide poisoning
occurs when carbon monoxide builds up in your bloodstream. When too much carbon
monoxide is in the air, your body replaces the oxygen in your red blood cells
with carbon monoxide. This can lead to serious tissue damage, or even death.
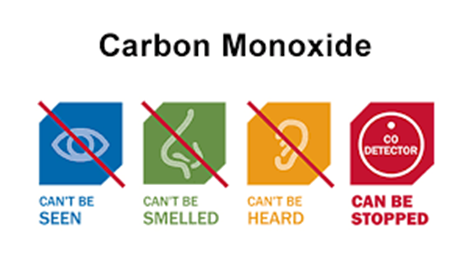
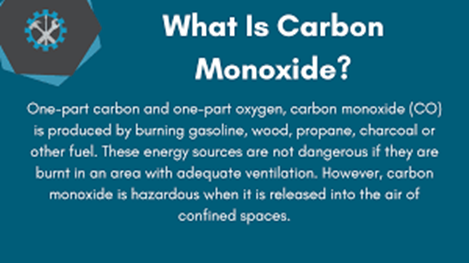
Carbon monoxide is a
colorless, odorless, tasteless gas produced by burning gasoline, wood, propane,
charcoal or other fuel. Improperly ventilated appliances and engines,
particularly in a tightly sealed or enclosed space, may allow carbon monoxide
to accumulate to dangerous levels.
If you think you or someone
you're with may have carbon monoxide poisoning, get into fresh air and seek
emergency medical care.
Symptoms
Signs and symptoms of carbon
monoxide poisoning may include:
Dull headache
Weakness
Dizziness
Nausea or vomiting
Shortness of breath
Confusion
Blurred vision
Loss of consciousness
Carbon monoxide poisoning
can be particularly dangerous for people who are sleeping or intoxicated. People
may have irreversible brain damage or even die before anyone realizes there's a
problem.
When to see a doctor
The warning signs of carbon
monoxide poisoning can be subtle. But the condition is a life-threatening
medical emergency. As stated above, if you
think you or someone you're with may have carbon monoxide poisoning, get into
fresh air and seek emergency medical care.
Causes
Carbon monoxide poisoning is
caused by inhaling combustion fumes. When too much carbon monoxide is in the
air you're breathing, your body replaces the oxygen in your red blood cells
with carbon monoxide. This prevents oxygen from reaching your tissues and
organs.
Various fuel-burning
appliances and engines produce carbon monoxide. The amount of carbon monoxide produced
by these sources usually isn't cause for concern. But if they're used in a
closed or partially closed space — cooking with a charcoal grill indoors, for
example — the carbon monoxide can build to dangerous levels.
Smoke inhalation during a
fire also can cause carbon monoxide poisoning.
Risk factors
Exposure to carbon monoxide
may be particularly dangerous for:
Unborn babies.
Fetal blood cells take up carbon monoxide more readily than adult blood cells
do. This makes unborn babies more susceptible to harm from carbon monoxide
poisoning.
Children.
Young children take breaths more frequently than adults do, which may make them
more susceptible to carbon monoxide poisoning.
Older adults.
Older people who experience carbon monoxide poisoning may be more likely to
develop brain damage.
People who have
chronic heart disease. People with a history of
anemia and breathing problems also are more likely to get sick from exposure to
carbon monoxide.
Those in whom carbon
monoxide poisoning leads to unconsciousness.
Loss of consciousness indicates more severe exposure.
Complications
Depending on the degree and
length of exposure, carbon monoxide poisoning can cause:
Permanent brain damage
Damage to your heart,
possibly leading to life-threatening cardiac complications
Fetal death or miscarriage
Death
Prevention
Simple precautions can help
prevent carbon monoxide poisoning:
Install carbon monoxide
detectors. Put one in the hallway near each sleeping area in your house. Check
the batteries every time you check your smoke detector batteries — at least
twice a year. If the alarm sounds, leave the house and call 911 or the fire
department. Carbon monoxide detectors are also available for motor homes and
boats.
Open the garage door before
starting your car. Never leave your car running in your garage. Be particularly
cautious if you have an attached garage. Leaving your car running in a space
attached to the rest of your house is never safe, even with the garage door
open.
Use gas appliances as
recommended. Never use a gas stove or oven to heat your home. Use portable gas
camp stoves outdoors only. Use fuel-burning space heaters only when someone is
awake to monitor them and doors or windows are open to provide fresh air. Don't
run a generator in an enclosed space, such as the basement or garage.
Keep your fuel-burning
appliances and engines properly vented. These include:
Space heaters
Furnaces
Charcoal grills
Cooking ranges
Water heaters
Fireplaces
Portable generators
Wood-burning stoves
Car and truck engines
Ask your utility company
about yearly checkups for all gas appliances, including your furnace.
If you have a fireplace,
keep it in good repair. Clean your fireplace chimney and flue every year.
Keep vents and chimneys
unblocked during remodeling. Check that they aren't covered by tarps or debris.
Make repairs before
returning to the site of a carbon
monoxide incident. If carbon monoxide
poisoning has occurred in your home, it's critical to find and repair the
source of the carbon monoxide before you stay there again. Your local fire
department or utility company may be able to help.
Use caution when working
with solvents in a closed area. Methylene chloride, a solvent commonly found in
paint and varnish removers, can break down (metabolize) into carbon monoxide
when inhaled. Exposure to methylene chloride can cause carbon monoxide
poisoning.
When working with solvents
at home, use them only outdoors or in well-ventilated areas. Carefully read the
instructions and follow the safety precautions on the label.
Jan Ricks Jennings, MHA, LFACHE
Senior Consultant
Senior Management Resources,
LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
March 20,2022