Atrial
fibrillation
Symptoms & causes
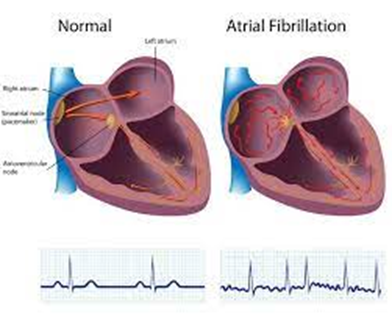
Atrial fibrillation (A-fib)
is an irregular and often very rapid heart rhythm (arrhythmia) that can lead to
blood clots in the heart. A-fib increases the risk of stroke, heart failure and
other heart-related complications.
During atrial fibrillation,
the heart's upper chambers (the atria) beat chaotically and irregularly — out
of sync with the lower chambers (the ventricles) of the heart. For many people,
A-fib may have no symptoms. However, A-fib may cause a fast, pounding heartbeat
(palpitations), shortness of breath or weakness.
Episodes of atrial
fibrillation may come and go, or they may be persistent. Although A-fib itself
usually isn't life-threatening, it's a serious medical condition that requires
proper treatment to prevent stroke.
Treatment for atrial
fibrillation may include medications, therapy to reset the heart rhythm and
catheter procedures to block faulty heart signals.
A person with atrial
fibrillation may also have a related heart rhythm problem called atrial
flutter. Although atrial flutter is a different arrhythmia, the treatment is
quite similar to atrial fibrillation.
Symptoms of a fast,
fluttering or pounding heartbeat (palpitations)
Chest pain
Dizziness
Fatigue
Lightheadedness
Reduced ability to exercise
Shortness of breath
Weakness
Atrial fibrillation may be:
Occasional
(paroxysmal atrial fibrillation). A-fib symptoms come and go, usually lasting
for a few minutes to hours. Sometimes symptoms occur for as long as a week and
episodes can happen repeatedly. Symptoms might go away on their own. Some people
with occasional A-fib need treatment.
Persistent.
With this type of atrial fibrillation, the heart rhythm doesn't go back to
normal on its own. If a person has A-fib symptoms, cardioversion or treatment
with medications may be used to restore and maintain a normal heart rhythm.
Long-standing persistent.
This type of atrial fibrillation is continuous and lasts longer than 12 months.
Permanent. In
this type of atrial fibrillation, the irregular heart rhythm can't be restored.
Medications are needed to control the heart rate and to prevent blood clots.
When to see a doctor
If you have any signs or
symptoms of atrial fibrillation, make an appointment with your doctor.
If you have chest pain, seek
immediate medical help. Chest pain could mean that you're having a heart attack
Causes
To understand the causes of
A-fib, it may be helpful to know how the heart typically beats.
The typical heart has four
chambers — two upper chambers (atria) and two lower chambers (ventricles).
Within the upper right chamber of the heart (right atrium) is a group of cells
called the sinus node. The sinus node is the heart's natural pacemaker. It
produces the signal that starts each heartbeat.
In a regular heart rhythm:
The signal travels from the
sinus node through the two upper heart chambers (atria).
The signal passes through a
pathway between the upper and lower chambers called the atrioventricular (AV)
node.
The movement of the signal
causes your heart to squeeze (contract), sending blood to your heart and body.
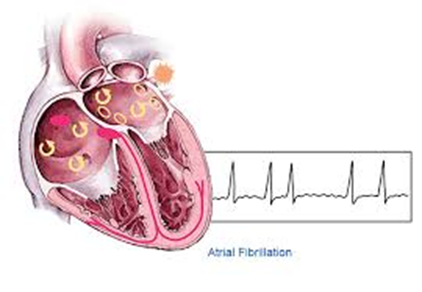
In atrial fibrillation, the
signals in the upper chambers of the heart are chaotic. As a result, the upper
chambers shake (quiver). The AV node is then bombarded with signals trying to
get through to the lower heart chambers (ventricles). This causes a fast and
irregular heart rhythm.
The heart rate in atrial
fibrillation may range from 100 to 175 beats a minute. The normal range for a
heart rate is 60 to 100 beats a minute.
Causes of atrial
fibrillation
Problems with the heart's
structure are the most common cause of atrial fibrillation. Possible causes of
atrial fibrillation include:
Coronary artery disease
Heart attack
Heart defect that you're
born with (congenital heart defect)
Heart valve problems
High blood pressure
Lung diseases
Physical stress due to
surgery, pneumonia or other illnesses
Previous heart surgery
Problem with the heart's
natural pacemaker (sick sinus syndrome)
Sleep apnea
Thyroid disease such as an
overactive thyroid (hyperthyroidism) and other metabolic imbalances
Use of stimulants, including
certain medications, caffeine, tobacco and alcohol
Viral infections
Some people who have atrial
fibrillation have no known heart problems or heart damage.
Risk factors
Things that can increase the
risk of atrial fibrillation (A-fib) include:
Age.
The older a person is, the greater the risk of developing atrial fibrillation.
Heart disease.
Anyone with heart disease — such as heart valve problems, congenital heart
disease, congestive heart failure, coronary artery disease, or a history of
heart attack or heart surgery — has an increased risk of atrial fibrillation.
High blood pressure.
Having high blood pressure, especially if it's not well controlled with
lifestyle changes or medications, can increase the risk of atrial fibrillation.
Thyroid disease. In
some people, thyroid problems may trigger heart rhythm problems (arrhythmias),
including atrial fibrillation.
Other chronic health
conditions. People with certain chronic conditions such as
diabetes, metabolic syndrome, chronic kidney disease, lung disease or sleep
apnea have an increased risk of atrial fibrillation.
Drinking alcohol.
For some people, drinking alcohol can trigger an episode of atrial
fibrillation. Binge drinking further increases the risk.
Obesity.
People who have obesity are at higher risk of developing atrial fibrillation.
Family history. An
increased risk of atrial fibrillation occurs in some families.
Complications
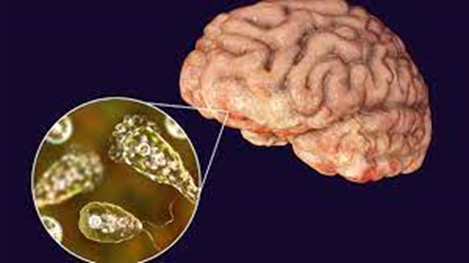
Blood clots are a dangerous
complication of atrial fibrillation that can lead to stroke.
In atrial fibrillation, the
chaotic heart rhythm can cause blood to collect in the heart's upper chambers
(atria) and form clots. If a blood clot in the left upper chamber (left atrium)
breaks free from the heart area, it can travel to the brain and cause a stroke.
The risk of stroke from
atrial fibrillation increases as you grow older. Other health conditions also
may increase your risk of a stroke due to A-fib, including:
High blood pressure
Diabetes
Heart failure
Some valvular heart disease
Blood thinners are commonly
prescribed to prevent blood clots and strokes in people with atrial
fibrillation.
Prevention
Healthy lifestyle choices
can reduce the risk of heart disease and may prevent atrial fibrillation. Here
are some basic heart-healthy tips:
Eat a nutritious diet
Get regular exercise and
maintain a healthy weight
Don't smoke
Avoid or limit alcohol and
caffeine
Manage stress, as intense
stress and anger can cause heart rhythm problems
Jan Ricks Jennings, MHA,
LFACHE
Senior Consultant
Senior Management Resources,
LLC
JanJenningsBlog.Blogspot.net
412.913.0636 Cell
724.733.0509 Office
May 30, 2022