Drug
addiction
Overview
Drug addiction, also called
substance use disorder, is a disease that affects a person's brain and behavior
and leads to an inability to control the use of a legal or illegal drug or
medication. Substances such as alcohol, marijuana and nicotine also are
considered drugs. When you're addicted, you may continue using the drug despite
the harm it causes.
Drug addiction can start
with experimental use of a recreational drug in social situations, and, for
some people, the drug use becomes more frequent. For others, particularly with
opioids, drug addiction begins with exposure to prescribed medications, or
receiving medications from a friend or relative who has been prescribed the
medication.
The risk of addiction and how
fast you become addicted varies by drug. Some drugs, such as opioid
painkillers, have a higher risk and cause addiction more quickly than others.
As time passes, you may need
larger doses of the drug to get high. Soon you may need the drug just to feel
good. As your drug use increases, you may find that it's increasingly difficult
to go without the drug. Attempts to stop drug use may cause intense cravings
and make you feel physically ill (withdrawal symptoms).
You may need help from your
doctor, family, friends, support groups or an organized treatment program to
overcome your drug addiction and stay drug-free
Symptoms
Drug addiction symptoms or
behaviors include, among others:
Feeling that you have to use
the drug regularly — daily or even several times a day
Having intense urges for the
drug that block out any other thoughts
Over time, needing more of
the drug to get the same effect
Taking larger amounts of the
drug over a longer period of time than you intended
Making certain that you
maintain a supply of the drug
Spending money on the drug,
even though you can't afford it
Not meeting obligations and
work responsibilities, or cutting back on social or recreational activities
because of drug use
Continuing to use the drug,
even though you know it's causing problems in your life or causing you physical
or psychological harm
Doing things to get the drug
that you normally wouldn't do, such as stealing
Driving or doing other risky
activities when you're under the influence of the drug
Spending a good deal of time
getting the drug, using the drug or recovering from the effects of the drug
Failing in your attempts to
stop using the drug
Experiencing withdrawal
symptoms when you attempt to stop taking the drug
Recognizing unhealthy
drug use in family members
Sometimes it's difficult to
distinguish normal teenage moodiness or angst from signs of drug use. Possible
indications that your teenager or other family member is using drugs include:
Problems at school or work —
frequently missing school or work, a sudden disinterest in school activities or
work, or a drop in grades or work performance
Physical health issues —
lack of energy and motivation, weight loss or gain, or red eyes
Neglected appearance — lack
of interest in clothing, grooming or looks
Changes in behavior —
exaggerated efforts to bar family members from entering his or her room or
being secretive about where he or she goes with friends; or drastic changes in
behavior and in relationships with family and friends
Money issues — sudden requests
for money without a reasonable explanation; or your discovery that money is
missing or has been stolen or that items have disappeared from your home,
indicating maybe they're being sold to support drug use
Recognizing signs of
drug use or intoxication
Signs and symptoms of drug
use or intoxication may vary, depending on the type of drug. Below you'll find
several examples.
Marijuana, hashish
and other cannabis-containing substances
People use cannabis by
smoking, eating or inhaling a vaporized form of the drug. Cannabis often
precedes or is used along with other substances, such as alcohol or illegal
drugs, and is often the first drug tried.
Signs and symptoms of recent
use can include:
A sense of euphoria or
feeling "high"
A heightened sense of visual,
auditory and taste perception
Increased blood pressure and
heart rate
Red eyes
Dry mouth
Decreased coordination
Difficulty concentrating or
remembering
Slowed reaction time
Anxiety or paranoid thinking
Cannabis odor on clothes or
yellow fingertips
Exaggerated cravings for
certain foods at unusual times
Long-term (chronic) use is
often associated with:
Decreased mental sharpness
Poor performance at school
or at work
Reduced number of friends
and interests
K2, Spice and bath
salts
Two groups of synthetic
drugs — synthetic cannabinoids and substituted or synthetic cathinones — are
illegal in most states. The effects of these drugs can be dangerous and
unpredictable, as there is no quality control and some ingredients may not be
known.
Synthetic cannabinoids, also
called K2 or Spice, are sprayed on dried herbs and then smoked, but can be
prepared as an herbal tea. Despite manufacturer claims, these are chemical
compounds rather than "natural" or harmless products. These drugs can
produce a "high" similar to marijuana and have become a popular but
dangerous alternative.
Signs and symptoms of recent
use can include:
A sense of euphoria or
feeling "high"
Elevated mood
An altered sense of visual,
auditory and taste perception
Extreme anxiety or agitation
Paranoia
Hallucinations
Increased heart rate and
blood pressure or heart attack
Vomiting
Confusion
Substituted cathinones, also
called "bath salts," are mind-altering (psychoactive) substances
similar to amphetamines such as ecstasy (MDMA) and cocaine. Packages are often
labeled as other products to avoid detection.
Despite the name, these are
not bath products such as Epsom salts. Substituted cathinones can be eaten,
snorted, inhaled or injected and are highly addictive. These drugs can cause
severe intoxication, which results in dangerous health effects or even death.
Signs and symptoms of recent
use can include:
Euphoria
Increased sociability
Increased energy and
agitation
Increased sex drive
Increased heart rate and
blood pressure
Problems thinking clearly
Loss of muscle control
Paranoia
Panic attacks
Hallucinations
Delirium
Psychotic and violent
behavior
Barbiturates,
benzodiazepines and hypnotics
Barbiturates,
benzodiazepines and hypnotics are prescription central nervous system
depressants. They're often used and misused in search for a sense of relaxation
or a desire to "switch off" or forget stress-related thoughts or
feelings.
Barbiturates.
Examples include phenobarbital and secobarbital (Seconal).
Benzodiazepines.
Examples include sedatives, such as diazepam (Valium), alprazolam (Xanax),
lorazepam (Ativan), clonazepam (Klonopin) and chlordiazepoxide (Librium).
Hypnotics.
Examples include prescription sleeping medications such as zolpidem (Ambien,
Intermezzo, others) and zaleplon (Sonata).
Signs and symptoms of recent
use can include:
Drowsiness
Slurred speech
Lack of coordination
Irritability or changes in
mood
Problems concentrating or
thinking clearly
Memory problems
Involuntary eye movements
Lack of inhibition
Slowed breathing and reduced
blood pressure
Falls or accidents
Dizziness
Meth, cocaine and
other stimulants
Stimulants include
amphetamines, meth (methamphetamine), cocaine, methylphenidate (Ritalin,
Concerta, others) and amphetamine-dextroamphetamine (Adderall, Adderall XR,
others). They are often used and misused in search of a "high," or to
boost energy, to improve performance at work or school, or to lose weight or
control appetite.
Signs and symptoms of recent
use can include:
Feeling of exhilaration and
excess confidence
Increased alertness
Increased energy and
restlessness
Behavior changes or
aggression
Rapid or rambling speech
Dilated pupils
Confusion, delusions and
hallucinations
Irritability, anxiety or
paranoia
Changes in heart rate, blood
pressure and body temperature
Nausea or vomiting with
weight loss
Impaired judgment
Nasal congestion and damage
to the mucous membrane of the nose (if snorting drugs)
Mouth sores, gum disease and
tooth decay from smoking drugs ("meth mouth")
Insomnia
Depression as the drug wears
off
Club drugs
Club drugs are commonly used
at clubs, concerts and parties. Examples include ecstasy or molly (MDMA),
gamma-hydroxybutyric acid (GHB), flunitrazepam (Rohypnol ― a brand used outside
the U.S. ― also called roofie) and ketamine. These drugs are not all in the
same category, but they share some similar effects and dangers, including
long-term harmful effects.
Because GHB and
flunitrazepam can cause sedation, muscle relaxation, confusion and memory loss,
the potential for sexual misconduct or sexual assault is associated with the
use of these drugs.
Signs and symptoms of use of
club drugs can include:
Hallucinations
Paranoia
Dilated pupils
Chills and sweating
Involuntary shaking
(tremors)
Behavior changes
Muscle cramping and teeth
clenching
Muscle relaxation, poor
coordination or problems moving
Reduced inhibitions
Heightened or altered sense
of sight, sound and taste
Poor judgment
Memory problems or loss of
memory
Reduced consciousness
Increased or decreased heart
rate and blood pressure
Hallucinogens
Use of hallucinogens can
produce different signs and symptoms, depending on the drug. The most common
hallucinogens are lysergic acid diethylamide (LSD) and phencyclidine (PCP).
LSD use may cause:
Hallucinations
Greatly reduced perception
of reality, for example, interpreting input from one of your senses as another,
such as hearing colors
Impulsive behavior
Rapid shifts in emotions
Permanent mental changes in
perception
Rapid heart rate and high
blood pressure
Tremors
Flashbacks, a re-experience
of the hallucinations — even years later
PCP use may cause:
A feeling of being separated
from your body and surroundings
Hallucinations
Problems with coordination
and movement
Aggressive, possibly violent
behavior
Involuntary eye movements
Lack of pain sensation
Increase in blood pressure
and heart rate
Problems with thinking and
memory
Problems speaking
Impaired judgment
Intolerance to loud noise
Sometimes seizures or coma
Inhalants
Signs and symptoms of
inhalant use vary, depending on the substance. Some commonly inhaled substances
include glue, paint thinners, correction fluid, felt tip marker fluid,
gasoline, cleaning fluids and household aerosol products. Due to the toxic
nature of these substances, users may develop brain damage or sudden death.
Signs and symptoms of use
can include:
Possessing an inhalant
substance without a reasonable explanation
Brief euphoria or
intoxication
Decreased inhibition
Combativeness or
belligerence
Dizziness
Nausea or vomiting
Involuntary eye movements
Appearing intoxicated with
slurred speech, slow movements and poor coordination
Irregular heartbeats
Tremors
Lingering odor of inhalant
material
Rash around the nose and
mouth
Opioid painkillers
Opioids are narcotic,
painkilling drugs produced from opium or made synthetically. This class of
drugs includes, among others, heroin, morphine, codeine, methadone and
oxycodone.
Sometimes called the
"opioid epidemic," addiction to opioid prescription pain medications
has reached an alarming rate across the United States. Some people who've been
using opioids over a long period of time may need physician-prescribed
temporary or long-term drug substitution during treatment.
Signs and symptoms of
narcotic use and dependence can include:
Reduced sense of pain
Agitation, drowsiness or
sedation
Slurred speech
Problems with attention and
memory
Constricted pupils
Lack of awareness or
inattention to surrounding people and things
Problems with coordination
Depression
Confusion
Constipation
Runny nose or nose sores (if
snorting drugs)
Needle marks (if injecting
drugs)
When to see a doctor
If your drug use is out of
control or causing problems, get help. The sooner you seek help, the greater
your chances for a long-term recovery. Talk with your primary doctor or see a
mental health professional, such as a doctor who specializes in addiction
medicine or addiction psychiatry, or a licensed alcohol and drug counselor.
Make an appointment to see a
doctor if:
You can't stop using a drug
You continue using the drug
despite the harm it causes
Your drug use has led to
unsafe behavior, such as sharing needles or unprotected sex
You think you may be having
withdrawal symptoms after stopping drug use
If you're not ready to
approach a doctor, help lines or hotlines may be a good place to learn about
treatment. You can find these lines listed on the internet or in the phone
book.
When to seek emergency help
Seek emergency help if you
or someone you know has taken a drug and:
May have overdosed
Shows changes in
consciousness
Has trouble breathing
Has seizures or convulsions
Has signs of a possible
heart attack, such as chest pain or pressure
Has any other troublesome
physical or psychological reaction to use of the drug
Staging an intervention
People struggling with
addiction usually deny that their drug use is problematic and are reluctant to
seek treatment. An intervention presents a loved one with a structured
opportunity to make changes before things get even worse and can motivate
someone to seek or accept help.
An intervention should be
carefully planned and may be done by family and friends in consultation with a
doctor or professional such as a licensed alcohol and drug counselor, or
directed by an intervention professional. It involves family and friends and
sometimes co-workers, clergy or others who care about the person struggling
with addiction.
During the intervention,
these people gather together to have a direct, heart-to-heart conversation with
the person about the consequences of addiction and ask him or her to accept
treatment.
Causes
Like many mental health
disorders, several factors may contribute to development of drug addiction. The
main factors are:
Environment.
Environmental factors, including your family's beliefs and attitudes and
exposure to a peer group that encourages drug use, seem to play a role in
initial drug use.
Genetics.
Once you've started using a drug, the development into addiction may be
influenced by inherited (genetic) traits, which may delay or speed up the
disease progression.
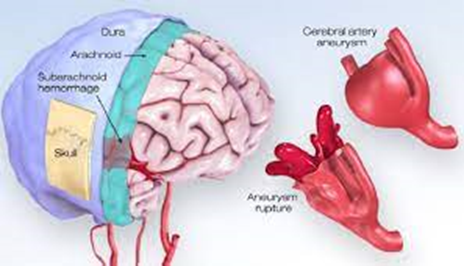
Changes in the brain
Physical addiction appears
to occur when repeated use of a drug changes the way your brain feels pleasure.
The addicting drug causes physical changes to some nerve cells (neurons) in
your brain. Neurons use chemicals called neurotransmitters to communicate.
These changes can remain long after you stop using the drug.
Risk factors
People of any age, sex or
economic status can become addicted to a drug. Certain factors can affect the
likelihood and speed of developing an addiction:
Family history of addiction.
Drug addiction is more common in some families and likely involves genetic
predisposition. If you have a blood relative, such as a parent or sibling, with
alcohol or drug addiction, you're at greater risk of developing a drug
addiction.
Mental health disorder. If
you have a mental health disorder such as depression,
attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress
disorder, you're more likely to become addicted to drugs. Using drugs can
become a way of coping with painful feelings, such as anxiety, depression and
loneliness, and can make these problems even worse.
Peer pressure. Peer pressure
is a strong factor in starting to use and misuse drugs, particularly for young
people.
Lack of family involvement.
Difficult family situations or lack of a bond with your parents or siblings may
increase the risk of addiction, as can a lack of parental supervision.
Early use. Using drugs at an
early age can cause changes in the developing brain and increase the likelihood
of progressing to drug addiction.
Taking a highly addictive
drug. Some drugs, such as stimulants, cocaine or opioid painkillers, may result
in faster development of addiction than other drugs. Smoking or injecting drugs
can increase the potential for addiction. Taking drugs considered less
addicting — so-called "light drugs" — can start you on a pathway of
drug use and addiction.
Complications
Drug use can have
significant and damaging short-term and long-term effects. Taking some drugs
can be particularly risky, especially if you take high doses or combine them
with other drugs or alcohol. Here are some examples.
Methamphetamine, opiates and
cocaine are highly addictive and cause multiple short-term and long-term health
consequences, including psychotic behavior, seizures or death due to overdose.
GHB and flunitrazepam may
cause sedation, confusion and memory loss. These so-called "date rape
drugs" are known to impair the ability to resist unwanted contact and
recollection of the event. At high doses, they can cause seizures, coma and
death. The danger increases when these drugs are taken with alcohol.
Ecstasy or molly (MDMA) can
cause dehydration, electrolyte imbalance and complications that can include
seizures. Long-term, MDMA can damage the brain.
One particular danger of
club drugs is that the liquid, pill or powder forms of these drugs available on
the street often contain unknown substances that can be harmful, including
other illegally manufactured or pharmaceutical drugs.
Due to the toxic nature of
inhalants, users may develop brain damage of different levels of severity.
Other life-changing
complications
Dependence on drugs can create
a number of dangerous and damaging complications, including:
Getting a communicable
disease. People who are addicted to a drug are more likely to get an infectious
disease, such as HIV, either through unsafe sex or by sharing needles.
Other health problems. Drug
addiction can lead to a range of both short-term and long-term mental and
physical health problems. These depend on what drug is taken.
Accidents. People who are
addicted to drugs are more likely to drive or do other dangerous activities
while under the influence.
Suicide. People who are
addicted to drugs die by suicide more often than people who aren't addicted.
Family problems. Behavioral
changes may cause marital or family conflict and custody issues.
Problems at school. Work
issues. Drug use can cause declining performance at work, absenteeism and
eventual loss of employment.
Problems Drug use can
negatively affect academic performance and motivation to excel in school.
Legal issues.
Legal problems are common for drug users and can stem from buying or possessing
illegal drugs, stealing to support the drug addiction, driving while under the
influence of drugs or alcohol, or disputes over child custody.
Financial problems.
Spending money to support drug use takes away money from other needs, could
lead to debt, and can lead to illegal or unethical behaviors.
Prevention
The best way to prevent an
addiction to a drug is not to take the drug at all. If your doctor prescribes a
drug with the potential for addiction, use care when taking the drug and follow
the instructions provided by your doctor.
Doctors should prescribe
these medications at safe doses and amounts and monitor their use so that
you're not given too great a dose or for too long a time. If you feel you need
to take more than the prescribed dose of a medication, talk to your doctor.
Preventing drug misuse in
children and teenagers
Take these steps to help
prevent drug misuse in your children and teenagers:
Communicate.
Talk to your children about the risks of drug use and misuse.
Listen. Be a good listener
when your children talk about peer pressure and be supportive of their efforts
to resist it.
Set a good example.
Don't misuse alcohol or addictive drugs. Children of parents who misuse drugs
are at greater risk of drug addiction.
Strengthen the bond.
Work on your relationship with your children. A strong, stable bond between you
and your child will reduce your child's risk of using or misusing drugs.
Preventing a relapse
Once you've been addicted to
a drug, you're at high risk of falling back into a pattern of addiction. If you
do start using the drug, it's likely you'll lose control over its use again —
even if you've had treatment and you haven't used the drug for some time.
Stick with your
treatment plan. Monitor your cravings. It may seem like
you've recovered and you don't need to keep taking steps to stay drug-free. But
your chances of staying drug-free will be much higher if you continue seeing
your therapist or counselor, going to support group meetings and taking
prescribed medication.
Avoid high-risk
situations. Don't go back to the neighborhood where you
used to get your drugs. And stay away from your old drug crowd.
Get help immediately
if you use the drug again. If you start using the drug
again, talk to your doctor, your mental health professional or someone else who
can help you right away.
Jan Ricks Jennings
Senior Consultant
Senior Management, Resources,
LLC
Jan.Jennings@EagleTalons.net
JanJenningsBlog.Blogspot.com
724.733.0509 Office
412.913.036 Cell
August 26, 2022