Rotavirus
Overview
Rotavirus is a very
contagious virus that causes diarrhea. Before the development of a vaccine,
most children had been infected with the virus at least once by age 5.
Although rotavirus
infections are unpleasant, you can usually treat this infection at home with
extra fluids to prevent dehydration. Occasionally, severe dehydration requires
receiving fluids through a vein (intravenously) in the hospital.
Good hygiene, such as
washing your hands regularly, is important. But vaccination is the best way to
prevent rotavirus infection.
Symptoms
A rotavirus infection
usually starts within two days of exposure to the virus. Early symptoms are a
fever and vomiting, followed by three to seven days of watery diarrhea. The
infection can cause abdominal pain as well.
In healthy adults, a
rotavirus infection may cause only mild signs and symptoms or none at all.
When to see a doctor
Call your child's doctor if
your child:
Has diarrhea for more than
24 hours
Vomits frequently
Has black or tarry stool or
stool containing blood or pus
Has a temperature of 102 F
(38.9 C) or higher
Seems tired, irritable or in
pain
Has signs or symptoms of
dehydration, including dry mouth, crying without tears, little or no urination,
unusual sleepiness, or unresponsiveness
If you're an adult, call
your doctor if you:
Can't keep liquids down for
24 hours
Have diarrhea for more than
two days
Have blood in your vomit or
bowel movements
Have a temperature higher
than 103 F (39.4 C)
Have signs or symptoms of
dehydration, including excessive thirst, dry mouth, little or no urination,
severe weakness, dizziness on standing, or lightheadedness
Causes
Rotavirus is present in an
infected person's stool two days before symptoms appear and for up to 10 days
after symptoms lessen. The virus spreads easily through hand-to-mouth contact
throughout this time — even if the infected person doesn't have symptoms.
If you have rotavirus and
you don't wash your hands after using the toilet — or your child has rotavirus
and you don't wash your hands after changing your child's diaper or helping
your child use the toilet — the virus can spread to anything you touch,
including food, toys and utensils. If another person touches your unwashed
hands or a contaminated object and then touches his or her mouth, an infection
may follow. The virus can remain infectious on surfaces that haven't been
disinfected for weeks or months.
It's possible to be infected
with rotavirus more than once, even if you've been vaccinated. However, repeat
infections are typically less severe.
Risk factors
Rotavirus infections are
common in children ages 3 to 35 months — particularly those who spend time in
child care settings. Older adults and adults caring for young children have an increased
risk of infection as well.
In the United States, the
risk of rotavirus is highest in winter and spring.
Complications
Severe diarrhea can lead to
dehydration, particularly in young children. Left untreated, dehydration can
become a life-threatening condition regardless of its cause.
Prevention
To reduce the spread of
rotavirus, wash your hands thoroughly and often — especially after you use the
toilet, change your child's diaper or help your child use the toilet. But even
strict hand-washing doesn't offer any guarantees. And commonly used alcohol-based
hand sanitizers have little effect on rotavirus.
The World Health
Organization recommends that all countries give infants a rotavirus vaccine.
There are two vaccines available:
RotaTeq. This vaccine is
given by mouth in three doses, often at 2, 4 and 6 months. The vaccine isn't
approved for use in older children or adults.
Rotarix. This vaccine is a
liquid given in two doses to infants at ages 2 months and 4 months.
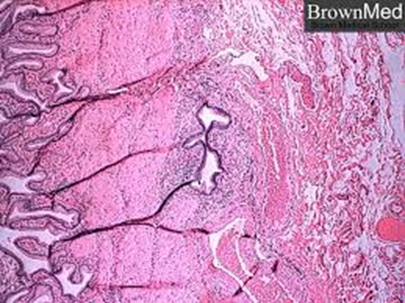
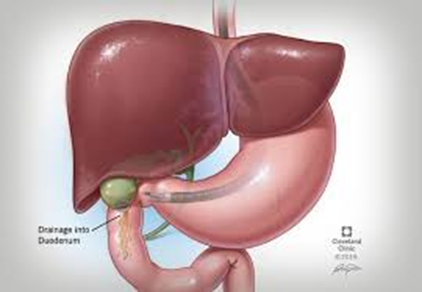
The vaccines are considered
safe and effective, and studies show that they prevent thousands of children
from developing rotavirus every year. However, rarely, they can cause a part of
the intestine to fold back on itself (intussusception), resulting in possibly
life-threatening intestinal blockage.
Children who have had
intussusception are more likely to have it again after receiving the rotavirus
vaccine. The U.S. Food and Drug Administration recommends that the vaccine not
be given to children who have a history of intussusception.
For children who don't have
a history of intussusception, there is a very small risk that it can develop
after the rotavirus vaccine is given. Even so, the benefits of the vaccine far
outweigh the risks.
If your child has stomach
pain, vomiting, diarrhea, blood in his or her stool, or a change in bowel
movements after getting the rotavirus vaccine, contact your doctor immediately.
Jan Ricks Jennings, MHA,
LFACHE
Senior Consultant
Senior Management
Resources, LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
412.913.0636 Cell
April 30, 2022