Abdominal Aortic Aneurysm
Overview
An aneurysm is a weak
section of an artery wall. Pressure from inside the artery causes the weakened
area to bulge out beyond the normal width of the blood vessel. An abdominal
aortic aneurysm is an aneurysm in the lower part of the aorta, the large artery
that runs through the torso.
Older, long-term smokers are
at especially high risk for abdominal aortic aneurysm.
Many people have no symptoms
and don’t know they have an aortic aneurysm until it ruptures, which is often
quickly fatal.
Symptoms, when they do
occur, include pain in the back or near the navel. An extremely sharp and
severe pain may indicate rupture, requiring emergency medical treatment.
Smaller, slow-growing aortic
aneurysms may be treated with watchful aneurysms may require surgery.
What is an abdominal
aortic aneurysm?
waiting, lifestyle changes
and medication. Large or fast-growing aortic
The aorta is the largest
blood vessel in the body. It delivers oxygenated blood from the heart to the rest
of the body. An aortic aneurysm is a bulging, weakened area in the wall of the
aorta. Over time, the blood vessel balloons and is at risk for bursting
(rupture) or separating (dissection). This can cause life threatening bleeding
and potentially death.
Aneurysms occur most often
in the portion of the aorta that runs through the abdomen (abdominal aortic
aneurysm). An abdominal aortic aneurysm is also called AAA or triple A. A
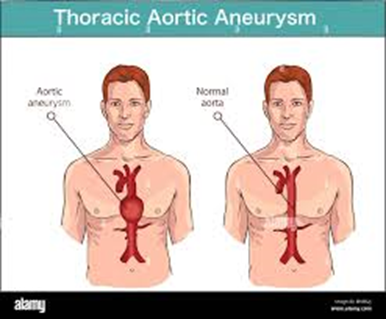
thoracic aortic aneurysm refers to the part of the aorta that runs through the
chest.
Once formed, an aneurysm
will gradually increase in size and get progressively weaker. Treatment for an
abdominal aneurysm may include surgical repair or removal of the aneurysm, or
inserting a metal mesh coil (stent) to support the blood vessel and prevent
rupture.
Abdominal Aortic Aneurysm
Shapes
Different types of aortic
aneurysms
The more common shape is
fusiform, which balloons out on all sides of the aorta. A bulging artery isn’t
classified as a true aneurysm until it increases the artery’s width by 50
percent.
A saccular shape is a bulge
in just one spot on the aorta. Sometimes this is called a pseudoaneurysm. It
usually means the inner layer of the artery wall is torn, which can be caused
by an injury or ulcer in the artery.
What causes an
abdominal aortic aneurysm to form?
Many things can cause the
breakdown of the aortic wall tissues and lead to an abdominal aortic aneurysm.
The exact cause isn't fully known. But, atherosclerosis is thought to play an
important role. Atherosclerosis is a buildup of plaque, which is a deposit of
fatty substances, cholesterol, cellular waste products, calcium, and fibrin in
the inner lining of an artery. Risk factors for atherosclerosis include:
Age (older than age 60)
Male (occurrence in males is
4 to 5 times greater than that of females)
Family history (first degree
relatives such as father or brother)
Genetic factors
High cholesterol
High blood pressure
Smoking
Diabetes
Obesity
Other diseases that may
cause an abdominal aneurysm include:
Connective tissue disorders
such as Marfan syndrome, Ehlers-Danlos syndrome, Turner's syndrome, and
polycystic kidney disease
Congenital (present at
birth) defects such as bicuspid aortic valve or coarctation of the aorta
Inflammation of the temporal
arteries and other arteries in the head and neck
Trauma
Infection such as syphilis,
salmonella, or staphylococcus (rare)
What are the symptoms of
abdominal aortic aneurysms?
About 3 out of 4 abdominal
aortic aneurysms don't cause symptoms. An aneurysm may be found by X-ray,
computed tomography (CT or CAT) scan, or magnetic resonance imaging (MRI) that
was done for other reasons. Since abdominal aneurysm may not have symptoms,
it's called the "silent killer" because it may rupture before being diagnosed.
Pain is the most common
symptom of an abdominal aortic aneurysm. The pain associated with an abdominal
aortic aneurysm may be located in the abdomen, chest, lower back, or groin
area. The pain may be severe or dull. Sudden, severe pain in the back or
abdomen may mean the aneurysm is about to rupture. This is a life-threatening
medical emergency.
Abdominal aortic aneurysms
may also cause a pulsing sensation, similar to a heartbeat, in the abdomen.
The symptoms of an abdominal
aortic aneurysm may look like other medical conditions or problems. Always see
your doctor for a diagnosis.
How are aneurysms
diagnosed?
Your doctor will do a
complete medical history and physical exam. Other possible tests include:
Computed tomography scan
(also called a CT or CAT scan). This test uses X-rays and computer technology
to make horizontal, or axial, images (often called slices) of the body. A CT
scan shows detailed images of any part of the body, including the bones,
muscles, fat, and organs. CT scans are more detailed than standard X-rays.
Magnetic resonance imaging
(MRI). This test uses a combination of large magnets, radiofrequencies, and a
computer to produce detailed images of organs and structures within the body.
Echocardiogram (also called
echo). This test evaluates the structure and function of the heart by using
sound waves recorded on an electronic sensor that make a moving picture of the
heart and heart valves, as well as the structures within the chest, such as the
lungs and the area around the lungs and the chest organs.
Transesophageal
echocardiogram (TEE). This test uses echocardiography to check for aneurysm,
the condition of heart valves, or presence of a tear of the lining of the
aorta. TEE is done by inserting a probe with a transducer on the end down the
throat.
Chest X-ray. This test uses
invisible electromagnetic energy beams to make images of internal tissues,
bones, and organs onto film.
Arteriogram (angiogram).
This is an X-ray image of the blood vessels that is used to assess conditions
such as aneurysm, narrowing of the blood vessel, or blockages. A dye (contrast)
will be injected through a thin, flexible tube placed in an artery. The dye
makes the blood vessels visible on an X-ray.
What is the treatment
for abdominal aortic aneurysms?
Treatment may include:
Monitoring with MRI or CT.
These tests are done to check the size and rate of growth of the aneurysm.
Managing risk factors.
Steps, such as quitting smoking, controlling blood sugar if you have diabetes,
losing weight if overweight, and eating a healthy diet may help control the
progression of the aneurysm.
Medicine. Used to control
factors such as high cholesterol or high blood pressure.
Surgery:
If the aneurysm is causing
symptoms or is large, your doctor may recommend surgery.
Surgery may be necessary if
the aneurysm is large or fast growing, increasing chances of rupture. Women
with large aneurysms are more likely than men to suffer a rupture.
Abdominal aortic aneurysm
open repair. A large incision is made in the abdomen to let the surgeon see and
repair the abdominal aorta aneurysm. A mesh, metal coil-like tube called a
stent or graft may be used. This graft is sewn to the aorta, connecting one end
of the aorta at the site of the aneurysm to the other end. The open repair is
the surgical standard for an abdominal aortic aneurysm.
Endovascular aneurysm repair
(EVAR). EVAR requires only small incisions in the groin. Using X-ray guidance
and specially-designed instruments, the surgeon can repair the aneurysm by
inserting the stent or graft inside the aorta. The graft material may cover the
stent. The stent helps hold the graft open and in place.
A small aneurysm or one that
doesn't cause symptoms may not require surgery until it reaches a certain size
or is rapidly increasing in size over a short period of time. Your doctor may
recommend "watchful waiting." This may include an ultrasound, duplex
scan, or CT scan every 6 months to closely monitor the aneurysm, and blood
pressure medicine may be used to control high blood pressure.
For suprarenal (above the
kidneys) AAA, only open surgery is available in the U.S. right now, though
Johns Hopkins vascular surgeons are involved in endovascular device trials that
may be a suitable option. However, AAA at or below the kidneys may be treated
by open or endovascular surgery. Endovascular means “within the blood vessel”
and is considered minimally invasive.
Not all patients can
tolerate the risk of open surgery, so endovascular repair is a great option.
Unfortunately, not all patients have the anatomy to qualify for endovascular
repair. Consult your vascular surgeon about which technique is best for you.
Stent graft repair of
abdominal aneurysm
Open aneurysm repair: A
large incision is made in the abdomen to repair the aneurysm. Another incision
is made in the aorta for the length of the aneurysm. A cylinder called a graft
is used for the repair. Grafts are made of polyester fabric or
polytetrafluoroethylene (PTFE, nontextile synthetic graft). This graft is sewn
to the aorta, from just above the aneurysm site to just below it. The artery
walls are then sewn over the graft.
Graft repair of abdominal
aneurysm
Endovascular aneurysm repair
(EVAR): A small incision is made in the groin. Using X-ray guidance, a stent
graft is inserted into the femoral artery and sent to the site of the aneurysm.
A stent is a thin metal mesh framework shaped into a long tube, while the
graft, a fabric covering the mesh, is made of a polyester fabric called PTFE.
The stent holds the graft open and in place.
EVAR is used only for an infrarenal (below the kidneys) AAA. It may be
more easily tolerated by high-risk patients. However, the graft can sometimes
slip out of place and may later need to be fixed.
Fenestrated stent graft for
abdominal aortic aneurysm
Fenestrated stent graft:
When the aneurysm is juxtarenal (at the kidneys) or involves the arteries of
the kidneys, the prior standard treatment has been open surgery. That’s because
a traditional stent graft has no openings to accommodate the branching of the
aorta to the kidneys. In 2012, the FDA approved a fenestrated stent graft, now
available in a few vascular surgery programs, including Johns Hopkins. The
fenestrated stent graft is made to the precise size of each patient’s aorta so
the openings for the renal (kidney) arteries are in just the right place to
maintain kidney circulation.
What is aortic
dissection?
An aortic dissection starts
with a tear in the inner layer of the aortic wall of the thoracic aorta. The
aortic wall is made up of 3 layers of tissue. When a tear occurs in the
innermost layer of the aortic wall, blood is then channeled into the wall of
the aorta separating the layers of tissues. This generates a weakening in the
aortic wall with a potential for rupture. Aortic dissection can be a
life-threatening emergency. The most commonly reported symptom of an aortic
dissection is sudden, severe, constant chest or upper back pain, sometimes
described as "ripping" or "tearing." The pain may move from
one place to another.
When a diagnosis of aortic
dissection is confirmed, immediate surgery or stenting is usually done.
What causes aortic
dissection?
The cause of aortic
dissection is unclear. However, several risk factors associated with aortic
dissection include:
High blood pressure
Connective tissue disorders,
such as Marfan's disease, Ehlers-Danlos syndrome, and Turner's syndrome
Cystic medial disease (a
degenerative disease of the aortic wall)
Aortitis (inflammation of
the aorta)
Atherosclerosis
Bicuspid aortic valve
(presence of only 2 cusps, or leaflets, in the aortic valve, rather than the
normal 3 cusps)
Trauma
Coarctation of the aorta
(narrowing of the aorta)
Excess fluid or volume in
the circulation (hypervolemia)
Polycystic kidney disease (a
genetic disorder characterized by the growth of numerous cysts filled with
fluid in the kidneys)
Jan Ricks Jennings, MHA ,
LFACHE
Senior Consultant
Senior Management Resources, LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
March 12, 2022



No comments:
Post a Comment