Anthrax
Anthrax is an infection
caused by the spore-forming bacteria called Bacillus anthracis. It is a
zoonosis (disease transmissible from animals to humans) that typically affects ruminants.
an even-toed ungulate mammal that chews the cud regurgitated from its rumen.
The ruminants comprise the cattle, sheep, antelopes, deer, giraffes, and their
relatives. (Such as cows, sheep, and goats). The bacteria produce extremely
potent toxins which are responsible for the symptoms, causing a high lethality
rate. Humans can catch the disease from infected animals or through
contaminated animal products.
Where is the disease
found?
The disease is present in
most parts of the world, but the frequency of outbreaks varies. Anthrax spores
may remain dormant in the soil for extended periods and resurface when the soil
is disturbed, such as by flooding, torrential rains, or landslides. The disease
typically reappears when grazing ruminants then ingest the spores.
How is the disease
transmitted?
Anthrax usually does not typically spread from animal to animal or human to human. When anthrax spores are ingested, inhaled, or enter the body through skin abrasions or cuts, they can germinate, multiply and produce toxin. Insects are an exception. They can transmit the bacterium between animals. Animal feed can be contaminated by anthrax if it contains bone meal of infected animals. Humans can get infected if they manage or participate in the slaughter of a sick animal or are in contact with contaminated animal products (such as meat, blood, wool, hides, bones). Anthrax can also be contracted in laboratory accidents. Furthermore, anthrax can be contracted by heroin-injecting drug-users through injection of contaminated heroin. Moreover, Bacillus anthracis has always been high on the list of potential agents of biological warfare and bioterrorism.
What are the clinical
presentations of anthrax in humans?
There are three forms of
anthrax in humans. Quick and appropriate medical evaluation and treatment are
essential for all three forms.
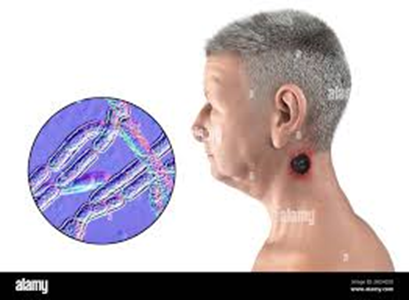
Cutaneous, or skin, anthrax
is the most generic form. It is usually contracted when a person with a break
in their skin, such as a cut or abrasion, comes into direct contact with
anthrax spores. The resulting itchy bump rapidly develops into a black sore.
Some people then develop headaches, muscle aches, fever, and vomiting.
Gastrointestinal anthrax is acquired
from eating meat from an infected animal. It causes initial symptoms like food
poisoning, but these can worsen to produce severe abdominal pain, vomiting of
blood and severe diarrhea.
The most severe, and rarest,
form of human anthrax is called inhalation or pulmonary anthrax. This form of
the disease is caused when a person is directly exposed to a large number of
anthrax spores suspended in the air, and breathes them in. The first symptoms
are like those of a common cold, but this can rapidly progress to severe breathing
difficulties and shock.
Can I catch anthrax from
another person?
In the case of cutaneous
anthrax, there is a small risk of direct infection from the lesions on another
person's body. Inhalation anthrax cannot be transmitted from person to person;
it can only be contracted by directly inhaling anthrax spores.
How is anthrax in
humans treated?
Hospitalization is required
for all human cases of anthrax. Individuals potentially exposed to anthrax
spores may be provided with prophylactic treatment. Anthrax responds well to
antibiotics, which need to be prescribed by a medical professional. Always
follow medical advice on how to take the antibiotics. Precisely follow the
instructions and do not shorten the course of treatment. Should any side
effects of the treatment be noted, please consult a physician at once. Nobody
should attempt to use antibiotics or any other drugs to treat or protect
themselves without first getting medical advice.
Is there a vaccine
for anthrax?
Anthrax vaccines for
livestock and humans exist. Veterinary vaccines are used for control of anthrax
in livestock. Human vaccines are in limited supply and used primarily for
protection of selected individuals with possible occupational exposure to
anthrax.
How can anthrax be
prevented?
Preventing the disease in
animals will protect human health. Breaking the cycle of infection is the basis
for control of anthrax in livestock. If a potential infectious source is known
to exist, this should be eliminated without delay.
In the event of a case or
outbreak occurring in livestock, control measures consist of correct disposal
of the carcass(es), decontamination of the site(s) and of items used to evaluate
and dispose of the carcass(es), of animals that have died from anthrax
initiation of treatment and/or vaccination of other animals as appropriate. The
best disposal method is incineration.
The carcass should not be opened since exposure to oxygen will allow the
bacteria to form spores.
Early detection of outbreaks,
quarantine of affected premises, destruction of diseased animals and fomites (objects
or materials which are likely to carry infection, such as clothes, utensils,
and furniture) and implementation of appropriate sanitary procedures at abattoirs
and dairy factories will ensure the safety of products of animal origin
intended for human consumption.
If a domestic animal
is sick or has just died, can its meat and hides be used?
Any animal that is sick,
behaves strangely or has died suddenly should not be used for food or for
making any product, as it may have succumbed to an infectious disease. Make
sure to follow national rules on veterinary inspection prior to slaughter as
these measures ensure food safety as well as safety of persons involved in the
slaughter.
Jan Ricks Jennings, Senior
Consultant
Senior Management Resources,
LLC
JanJenningsBlog.Blogspot.com
412.913.0636 Cell
724.733.0509 Office
January 10, 2022



No comments:
Post a Comment